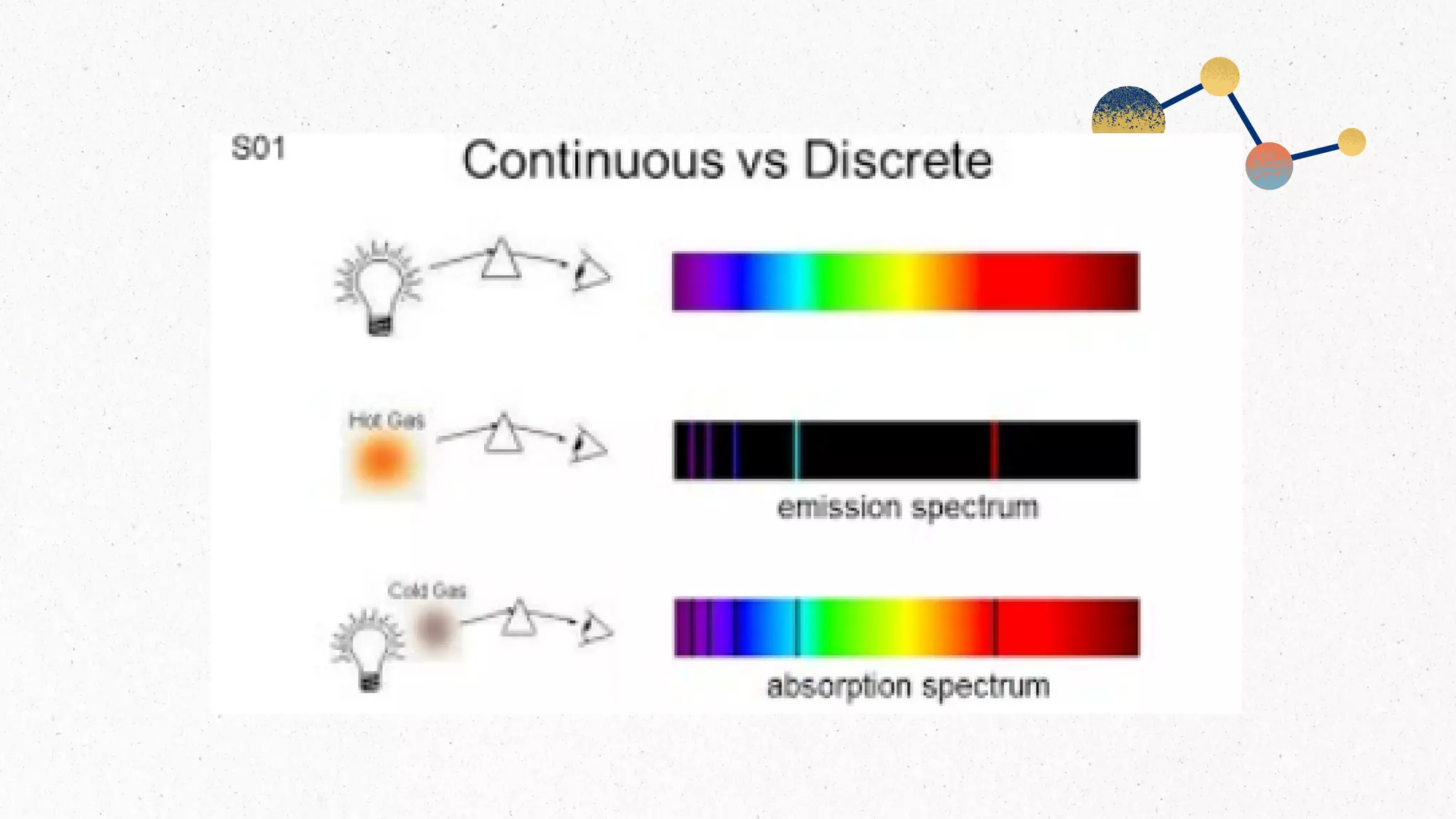
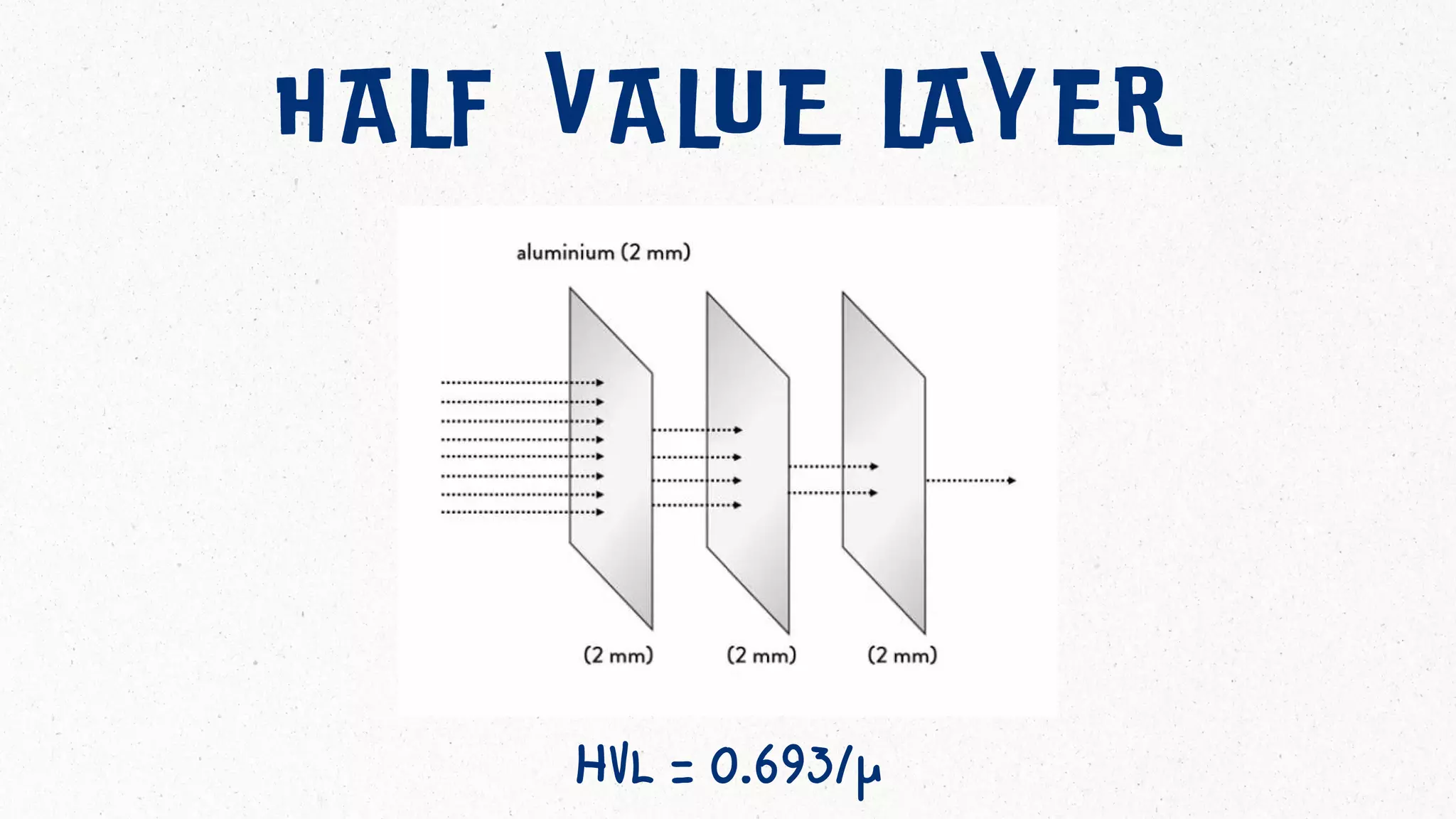
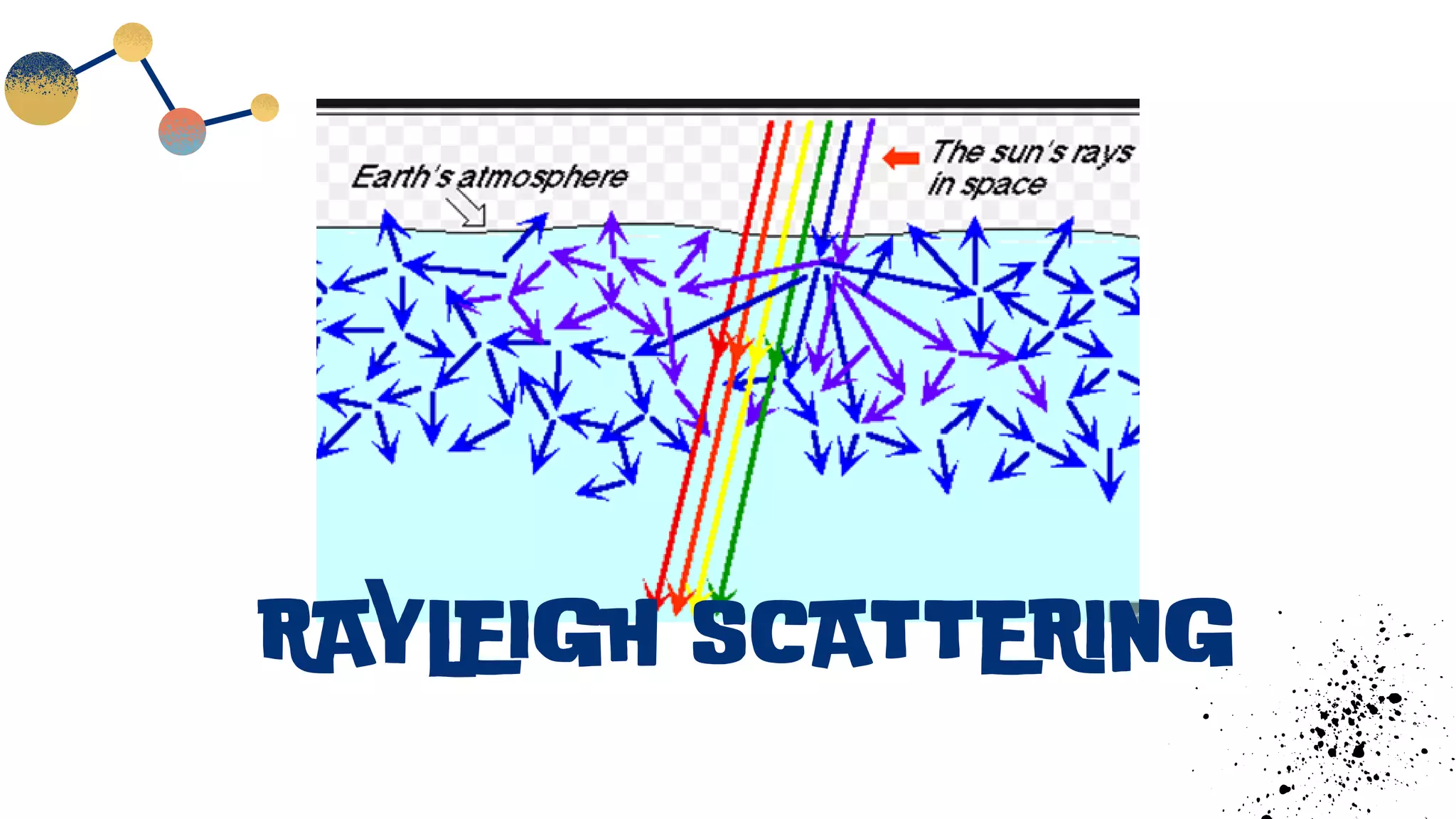
This document discusses x-ray interactions with matter. It begins by explaining the different types of x-ray emission spectra: bremsstrahlung or continuous spectrum which consists of photons of all energies emitted continuously, and characteristic spectrum which consists of photons with discrete energies. It then discusses various x-ray interaction processes with matter including Thomson scattering, Rayleigh scattering, attenuation, and the half value layer. It defines key terms like the linear and mass attenuation coefficients and explains their relationships to thickness and intensity reduction of the x-ray beam passing through materials.