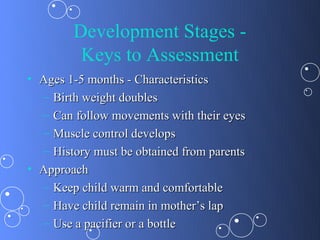
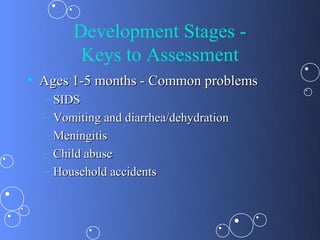
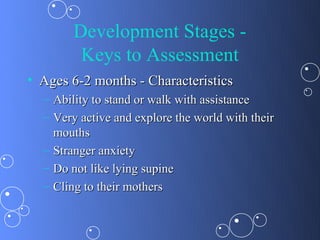
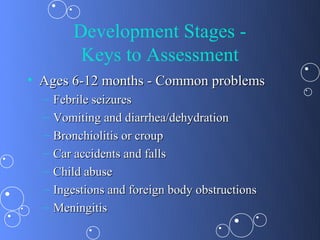
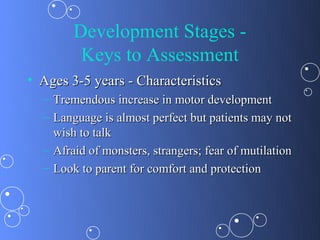
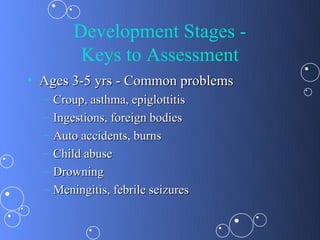
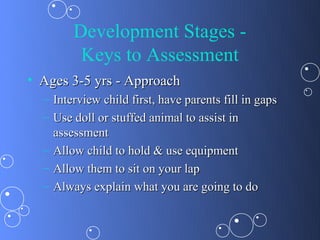
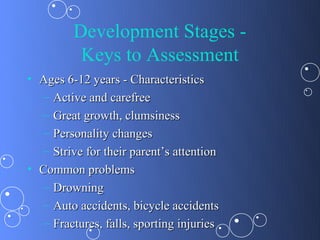
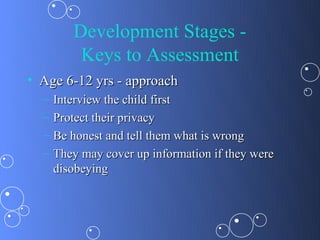
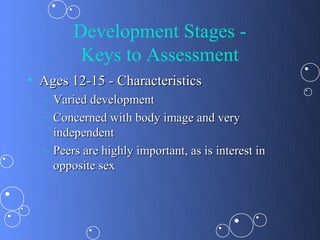
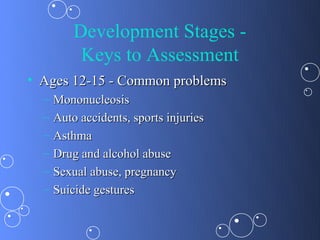
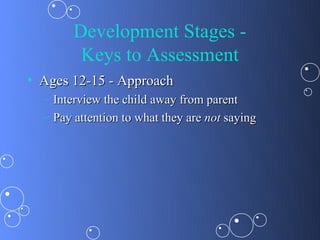
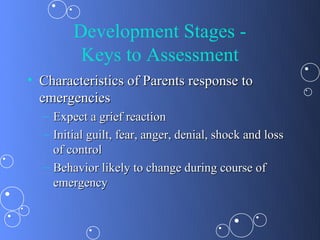
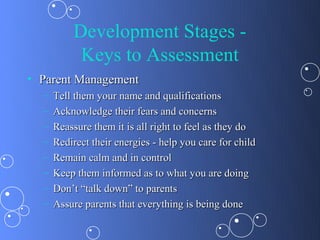
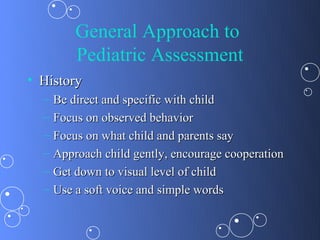
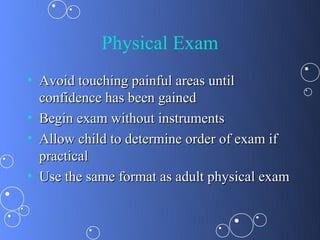
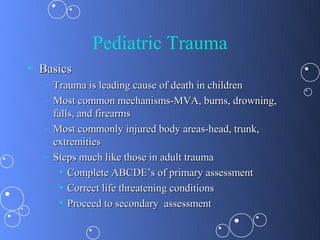
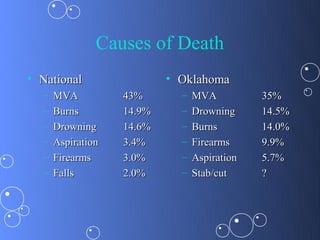
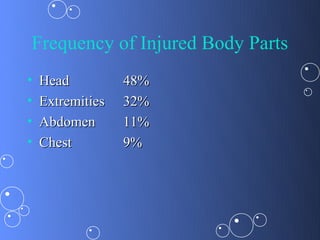
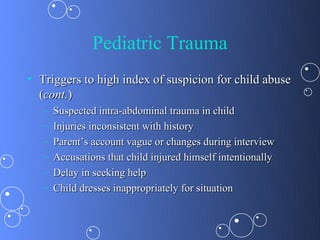
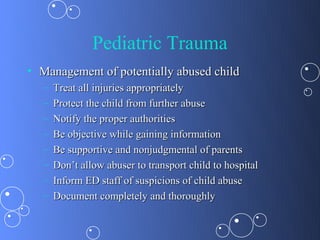
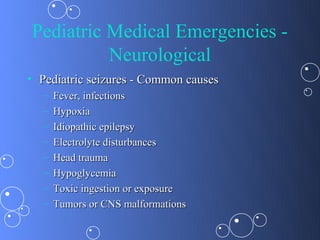
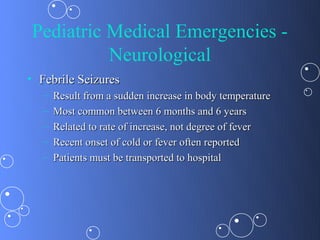
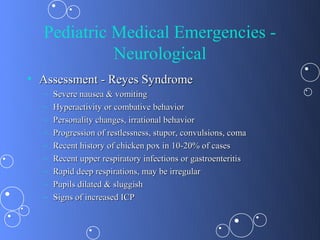
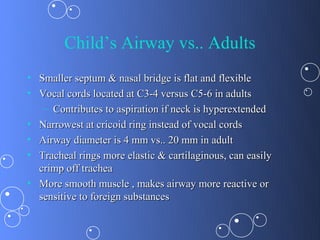
This document provides information on approaches to pediatric emergencies. It discusses assessing children of different ages, from neonates to adolescents. Common medical issues are reviewed for each age group. The document also covers pediatric trauma, including abuse assessment, and neurological emergencies like seizures, meningitis, and Reye's syndrome. Responding to pediatric emergencies requires developmentally appropriate approaches and consideration of age-specific illnesses and injuries.