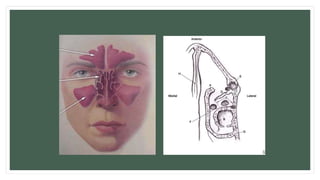
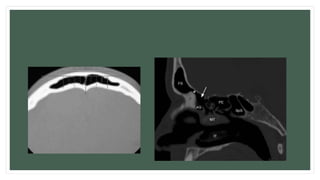
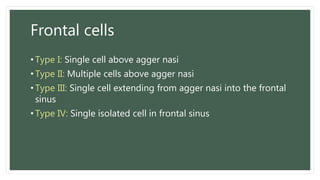
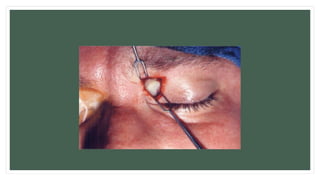
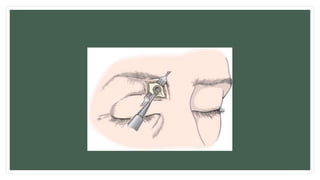
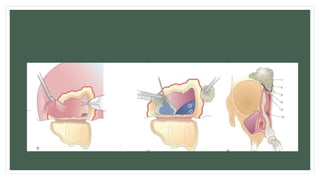
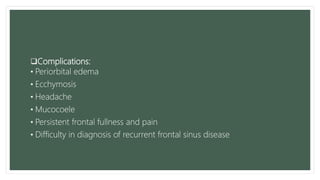
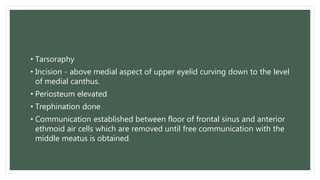
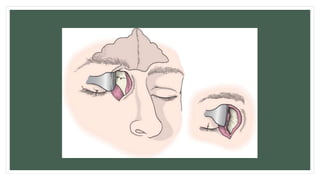
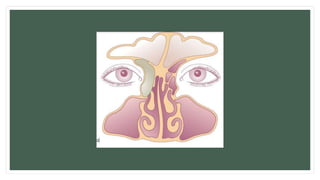
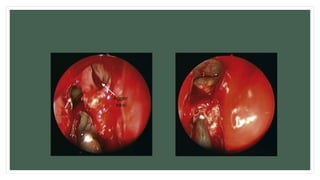
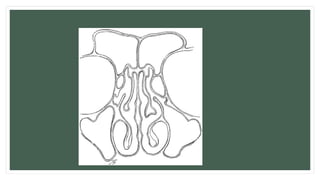
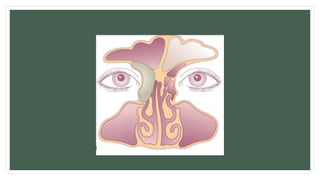
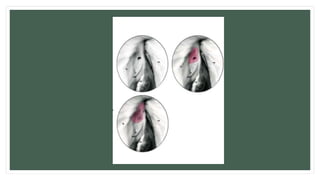
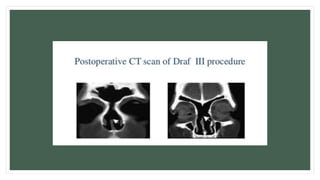
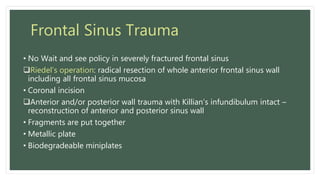
The document discusses surgical approaches for frontal sinus conditions. It describes the anatomy of the frontal sinus and various open and endoscopic surgical procedures for treating chronic sinusitis, trauma, tumors, and other indications. Open approaches include trephination, frontal sinusotomy, and ablation. Endoscopic approaches include DRAF types I-III. Complications and considerations for each procedure are also outlined.