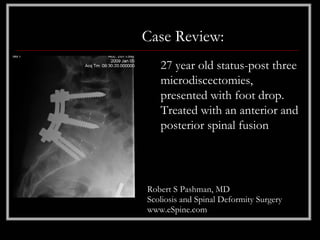
A 27-year-old female patient, post three microdiscectomies, presented with foot drop and significant low back pain due to ongoing lumbar spine issues. Following comprehensive surgery involving anterior and posterior spinal fusion, she regained strength and has been pain-free, ultimately leading to a successful pregnancy a year post-operation. The case highlights her transition from severe motor deficits to a successful outcome after advanced surgical intervention.