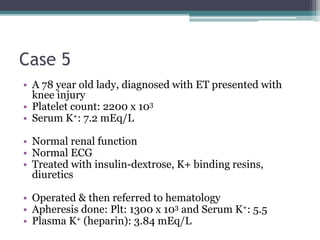
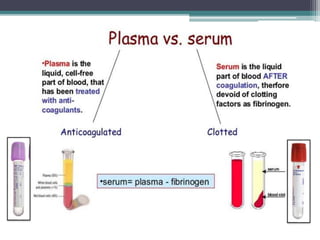
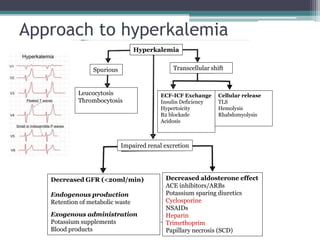
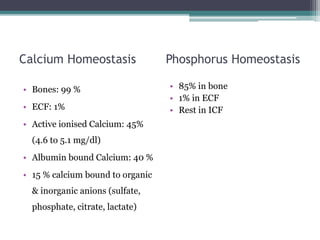
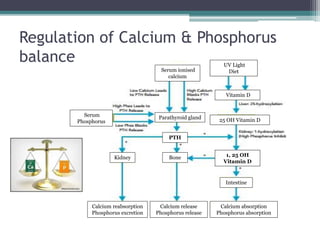
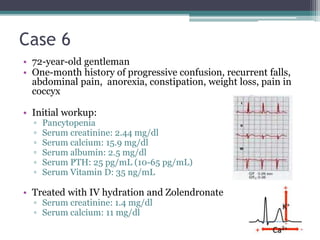
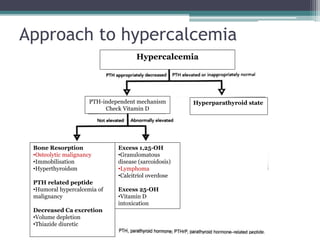
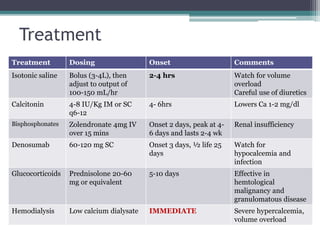
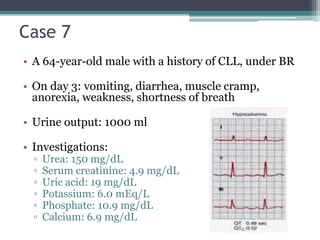
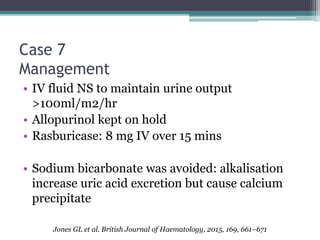
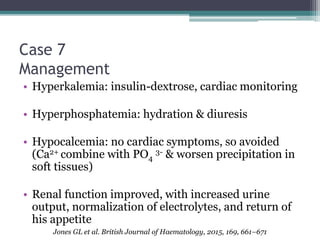
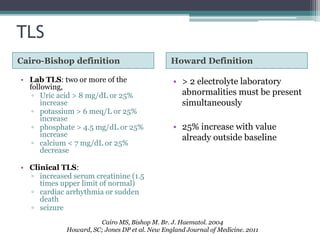
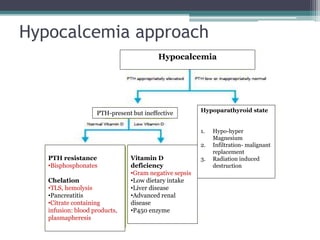
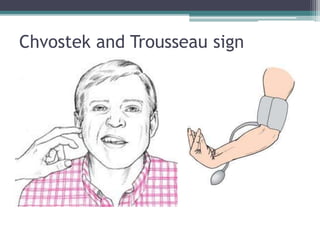
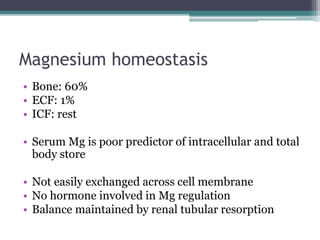
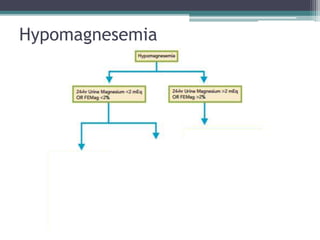
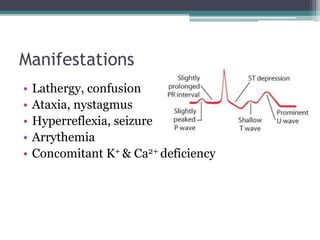
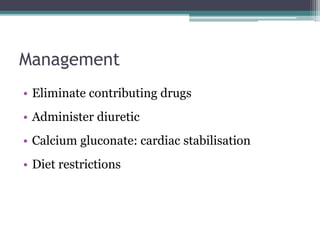
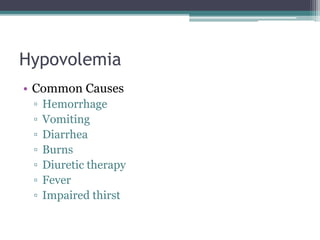
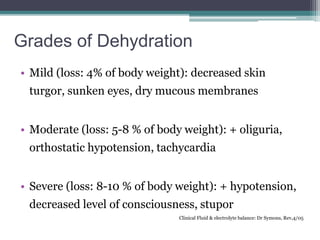
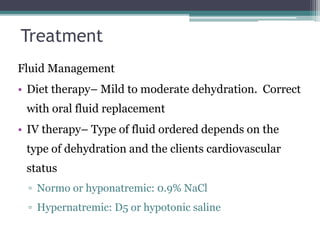
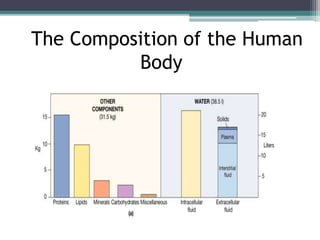
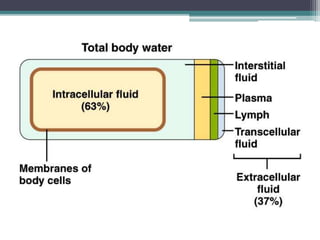
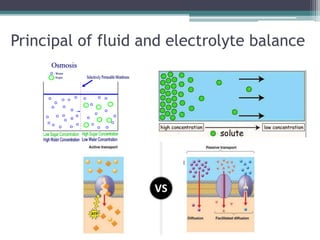
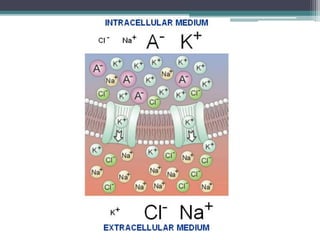
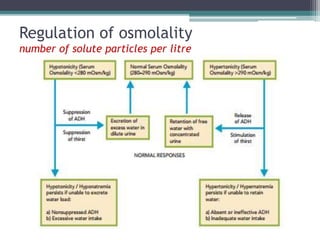
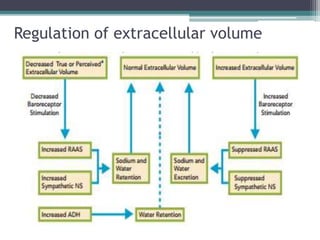
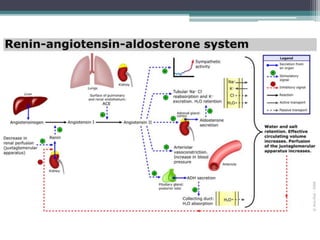
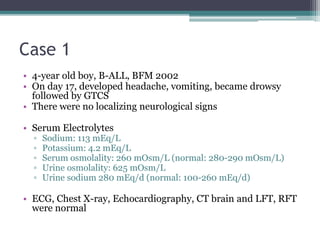
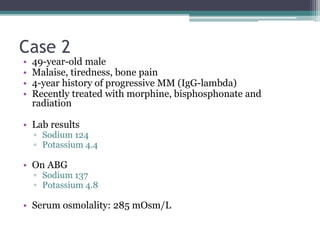
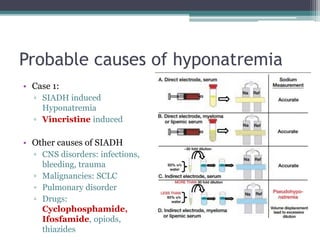
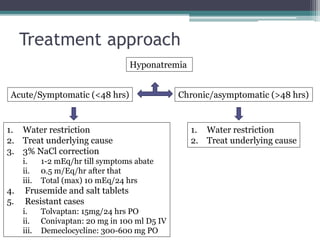
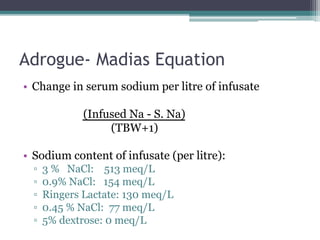
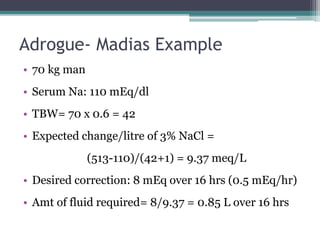
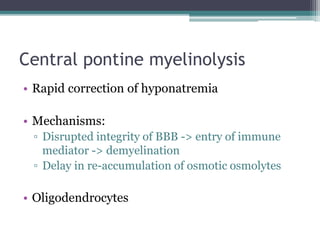
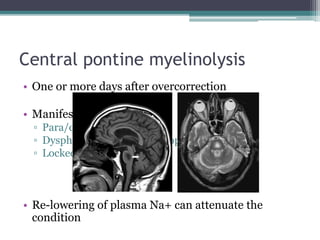
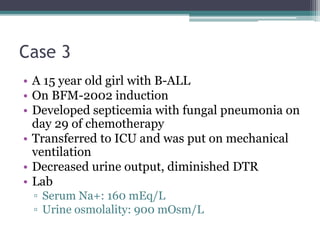
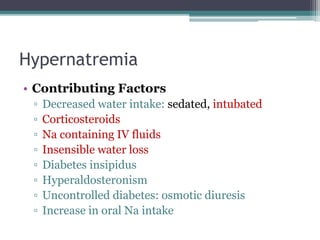
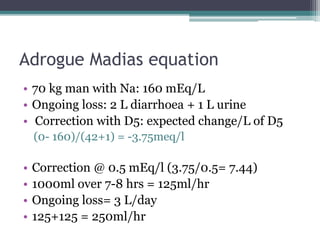
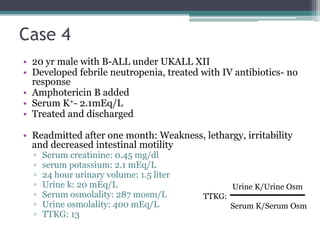
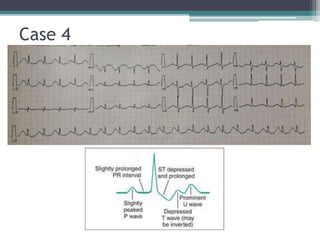
This document discusses fluid and electrolyte imbalances in hematology patients. It begins with basic concepts of fluid and electrolyte balance including osmolality, osmolarity, and their regulation. It then presents seven case studies demonstrating different electrolyte abnormalities - hyponatremia, pseudohyponatremia, hypernatremia, hypokalemia, hyperkalemia, hypercalcemia, and tumor lysis syndrome. For each case, it analyzes the abnormality, considers potential causes, and outlines treatment approaches. The document provides an in-depth review of fluid and electrolyte regulation and an approach to managing related clinical issues in hematology patients.
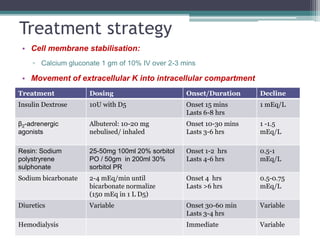
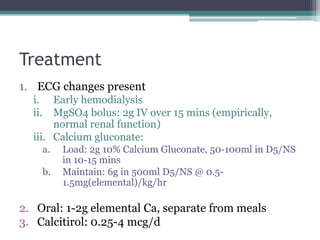
![Treatment
• Stop diuretics
• Correct Magnesium
• K+ replacement (IV or PO)
• (Body wt x Deficit x 0.4 [correction factor]) + body wt
• IV: ECG monitoring
• Encourage potassium-rich foods
▫ Normotensive: oral KCl
▫ Hypertensive: K+ sparing diuretics
• Treat underlying cause](https://image.slidesharecdn.com/fluidelectrolytebalance-170830170704/85/Fluid-electrolyte-balance-29-320.jpg)