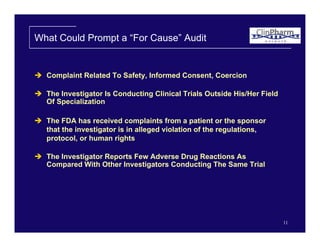
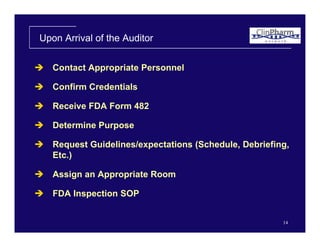
The document discusses the FDA's perspective on conducting inspections of clinical trial sites. It describes the goals of FDA inspections as assessing adherence to regulations and confirming safety and ethical treatment of subjects. The FDA conducts three types of inspections: trial oriented, investigator oriented, and bioequivalence inspections. Routine inspections provide advance notice while "for cause" inspections have no notice. Inspections involve reviewing documents, interviewing staff, and inspecting facilities. Common deficiencies found include inaccurate records, failure to follow protocols, and inadequate informed consent processes.