This document discusses maxillofacial infection, including:
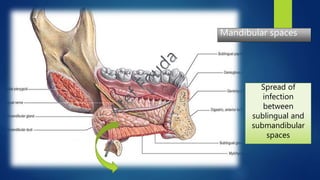
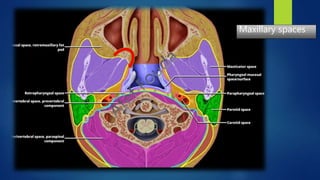
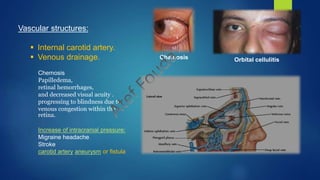
- The fascial spaces of the maxillofacial region and how infection can spread between them.
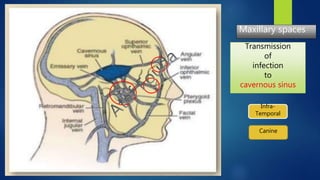
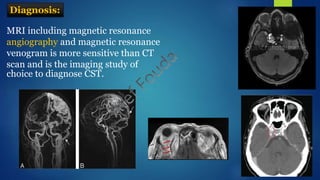
- Neurological complications of maxillofacial infection, especially cavernous sinus thrombosis which can cause issues like sensory deficits, eye movement problems, and increased intracranial pressure.
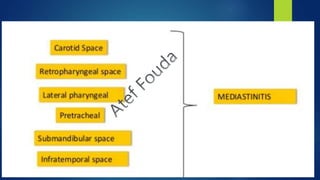
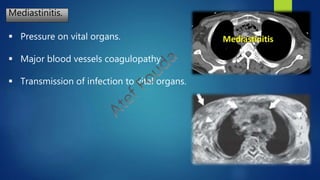
- Potentially fatal complications if the infection spreads to dangerous areas like the mediastinum or retroperitoneal spaces.















![ Mediastinal
infection
[vital organs].
Lateral pharyngeal
space infection
[vascular problems]
Submandibular-Sublingual-Submental
[Air-way].
Fatal complications of maxillofacial infection
Canine-Infratemporal
Neurological & [Brain damage].](https://image.slidesharecdn.com/docinfection-181016155934/85/Fatal-maxillofac-infection-19-320.jpg)

![Cavernous sinus thrombosis
Neurological manifestations:
Sensory deficits [V1 & V2]
Ophthalmic nerve.
Maxillary nerve.
Hypoesthesia or hyperesthesia of
the ophthalmic and maxillary
branch of the fifth nerve is
common.
Periorbital sensory loss and
impaired corneal reflex.](https://image.slidesharecdn.com/docinfection-181016155934/85/Fatal-maxillofac-infection-22-320.jpg)
![Cavernous sinus thrombosis
Neurological manifestations:
Motor cranial nerves:
Oculomotor nerve.[III]
Trochlear nerve. [IV]
Abducent nerve. [VI]](https://image.slidesharecdn.com/docinfection-181016155934/85/Fatal-maxillofac-infection-23-320.jpg)
![Cavernous sinus thrombosis
Eyelid drooping (ptosis)
pupil dilation (mydriasis)
Oculomotor nerve.[III]
ptosis
Mydriasis
Trochlear nerve. [IV]
Abducent nerve. [VI]
Diplopia](https://image.slidesharecdn.com/docinfection-181016155934/85/Fatal-maxillofac-infection-24-320.jpg)

![Anticoagulant:
Early heparinization [to achieve an INR of 2 to 3]
• Intracranial hemorrhage should first be ruled out before initiating heparin therapy.
Unilateral affection.
Steroid therapy helpful when progression to pituitary insufficiency
occurs.
Steroid
•Vancomycin plus ceftriaxone.
•Metronidazole IV should be added if anaerobic bacterial infection is suspected
(dental or sinus infection).
Antimicrobials
Treatment:](https://image.slidesharecdn.com/docinfection-181016155934/85/Fatal-maxillofac-infection-28-320.jpg)



![Complications
Carotid artery rupture.
Jugular vein coagulopathy.
Retropharyngeal extension [dangerous space].
Necrotizing fasciitis.
Carotid artery angiography](https://image.slidesharecdn.com/docinfection-181016155934/85/Fatal-maxillofac-infection-32-320.jpg)
![Retropharyngeal extension [dangerous space]
Retropharyngeal space
is the continuation of
Lateral(para)pharyngeal
space
and
Infratemporal space](https://image.slidesharecdn.com/docinfection-181016155934/85/Fatal-maxillofac-infection-33-320.jpg)


![Lab investigations.
Blood cell count.
Culture and sensitivity.
C-reactive protein.
PCR [New].
Imaging.
X-ray.
MRI
C.T
Ultra-sound.
Diagnostic aids:](https://image.slidesharecdn.com/docinfection-181016155934/85/Fatal-maxillofac-infection-37-320.jpg)
![Drawbacks of culture and sensitivity testing:
4-Delayed treatment [72 hours].
5-Economic status of the patient not taken into consideration.[price of antibiotic].
6-Errors of sampling may affect results.
7-Viral and fungal infections may be neglected.
8-Change of domain infective organism by time.
9-Most of viral infections couldn’t be cultured.
10-Systemic conditions of the patient may interfere with the results.
11-Availability of antibiotic should be taken into consideration.
12-Quality depend on the laboratory procedure.
1-Couldn’t test the ability of the antibiotic to reach the site of infection.
2-Host's immune system may affect antibiotic selected [bactericidal-bacteriostatic].
3-Problem of mixed infection.](https://image.slidesharecdn.com/docinfection-181016155934/85/Fatal-maxillofac-infection-38-320.jpg)


![genetic testing can be used to detect genes in the microorganism that cause resistance to certain
antimicrobial drugs Methicillin-Resistant Staphylococcus Aureus (MRSA) bacteria can be identified by
testing for the bacterial genes.
If a microorganism is difficult to culture or identify by other methods, doctors can do tests to identify
pieces of the microorganism’s genetic material. This genetic material consists of nucleic acids:
deoxyribonucleic acid (DNA) or ribonucleic acid (RNA).
The polymerase chain reaction (PCR) is an example of this type of test. The PCR technique is used to
produce many copies of a gene from a microorganism, making the microorganism much easier to identify.
Most nucleic acid–based tests are designed to identify the presence of a microorganism (called qualitative
testing). However, a few of these tests can measure the amount of genetic material present (called
quantitative testing) in certain microorganisms, such as HIV and hepatitis C, and thus determine how
severe the infection is. Quantitative tests can also be used to monitor how well treatment is
working[prognosis].
New trends in diagnosis:
Polymerase chain reaction [PCR].](https://image.slidesharecdn.com/docinfection-181016155934/85/Fatal-maxillofac-infection-41-320.jpg)
![New trends in diagnosis:
Polymerase chain reaction [PCR].](https://image.slidesharecdn.com/docinfection-181016155934/85/Fatal-maxillofac-infection-42-320.jpg)
![New trends in diagnosis:
Polymerase chain reaction [PCR].
Infectious disease applications:
• PCR allows for rapid and highly specific diagnosis of infectious diseases, including those
caused by bacteria or viruses.
• PCR also permits identification of non-cultivatable or slow-growing microorganisms such
as mycobacteria, anaerobic bacteria, or viruses from tissue culture.
• Some organisms are difficult to sample from patients and slow to be grown in the
laboratory[T.B] . PCR-based tests have allowed detection of small numbers of disease
organisms (both live or dead), in convenient samples.
• PCR tests have been developed that can detect as little as one viral genome. Infections can
be detected earlier.](https://image.slidesharecdn.com/docinfection-181016155934/85/Fatal-maxillofac-infection-43-320.jpg)
![• Donated blood can be screened directly for the virus.
• Detailed genetic analysis can also be used to detect antibiotic resistance, allowing
immediate and effective therapy.
• The spread of a disease organism through populations can be monitored by PCR testing.
• In many cases, the appearance of new virulent sub-types can be detected and monitored.
• The high sensitivity of PCR permits virus detection soon after infection and even before
the onset of disease. Such early detection may give physicians a significant lead time in
treatment. The amount of virus in a patient can also be quantified by PCR-based DNA
quantitation techniques.
New trends in diagnosis:
Polymerase chain reaction [PCR].
Infectious disease applications:](https://image.slidesharecdn.com/docinfection-181016155934/85/Fatal-maxillofac-infection-44-320.jpg)
![In modern laboratories, bacteria are usually identified by
characterization of the genome: identifying the characteristics of the
DNA and RNA of a sample species. This type of testing is generally
considered more reliable (and soon, less expensive) than actually
growing bacterial cultures and exposing them to various types of
antibiotics to see which drugs kill or inhibit the bacterial growth.
New trends in diagnosis:
Polymerase chain reaction [PCR].
Infectious disease applications:
• Expensive, not widely available.
• Each genetic test is specific to only one specific microorganism.](https://image.slidesharecdn.com/docinfection-181016155934/85/Fatal-maxillofac-infection-45-320.jpg)

