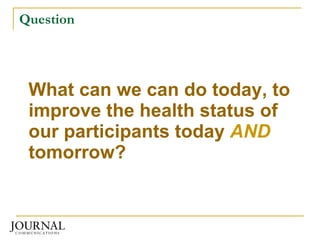
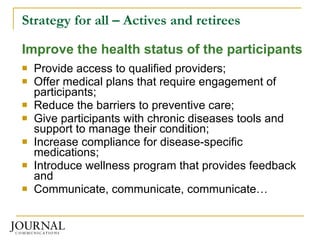
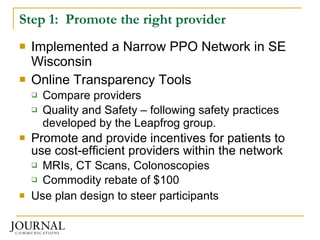
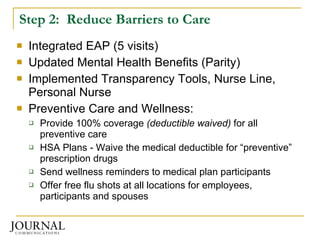
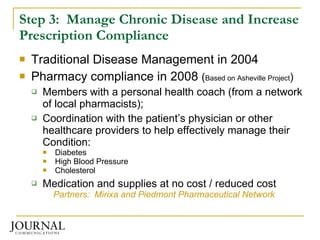
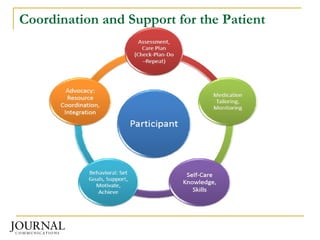
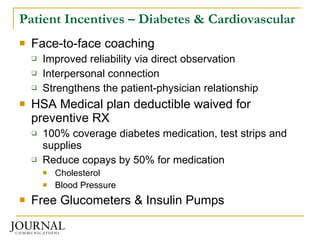
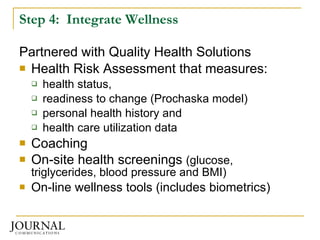
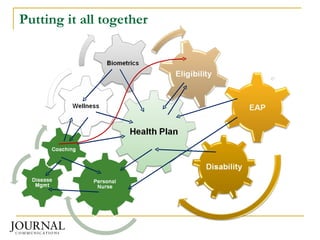
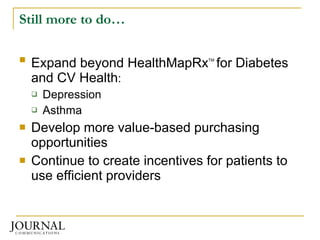
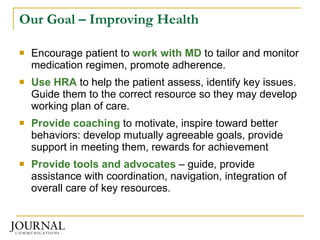
Journal Communications implemented a value-based benefit design to improve health outcomes and control costs. They promoted high-quality, low-cost providers and reduced barriers to preventive care. They also managed chronic diseases through a pharmacy compliance program offering coaching and incentives. Wellness programs were integrated, using data to connect participants with the right resources and motivate healthy behaviors. Through engagement and prevention, they achieved better health outcomes while lowering healthcare spending.

![Resources - Connections Center for Health Value Innovation Cyndy Nayer 314-422-4385, [email_address] Mirixa (HealthMapRx) Cindy Schaller, 703.865.2035, [email_address] www.HealthMapRx.com Piedmont Pharmaceutical Care Network Larry S. Long RPh, 336-202-7146, [email_address] Quality Health Solutions Brian J. Thomas, 888-747-0708 ext 102, [email_address]](https://image.slidesharecdn.com/evalu872009-12501789703221-phpapp03/85/Evalu8-72009-27-320.jpg)
![Questions? Christine Reichardt [email_address] 414-224-2069](https://image.slidesharecdn.com/evalu872009-12501789703221-phpapp03/85/Evalu8-72009-28-320.jpg)