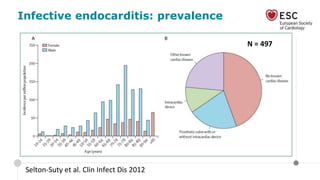
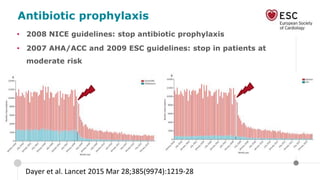
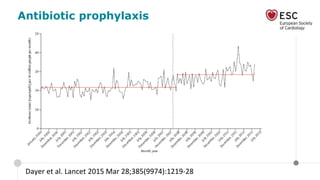
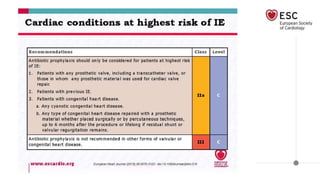
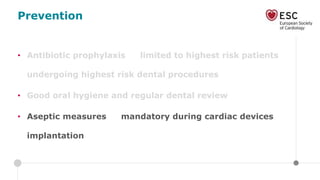
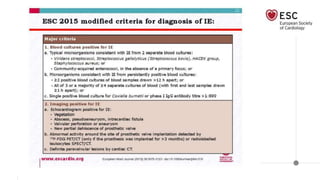
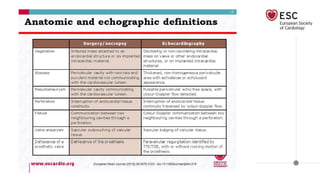
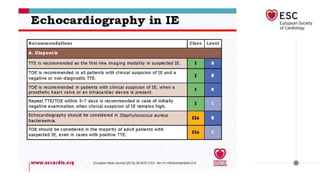
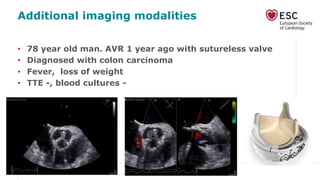
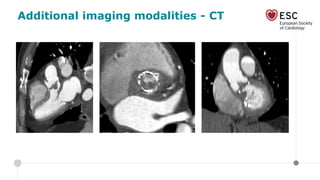
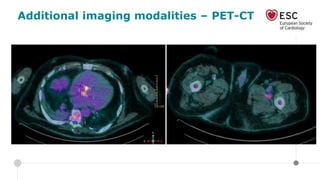
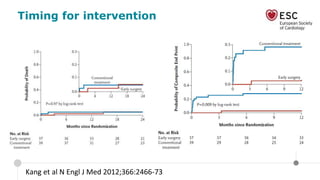
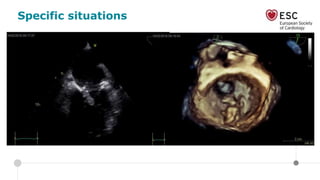
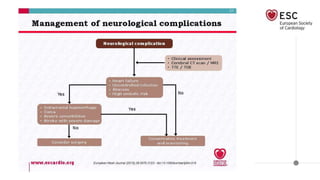
This document discusses infective endocarditis, including its prevalence, mortality rate, prevention, diagnosis, treatment, and timing of intervention. It provides an overview of antibiotic prophylaxis guidelines and limitations. Case examples are presented to demonstrate diagnostic imaging modalities like CT and PET-CT. The importance of an infective endocarditis team approach involving multiple specialties is highlighted. Specific clinical situations that require emergent versus urgent versus elective surgery are also examined.