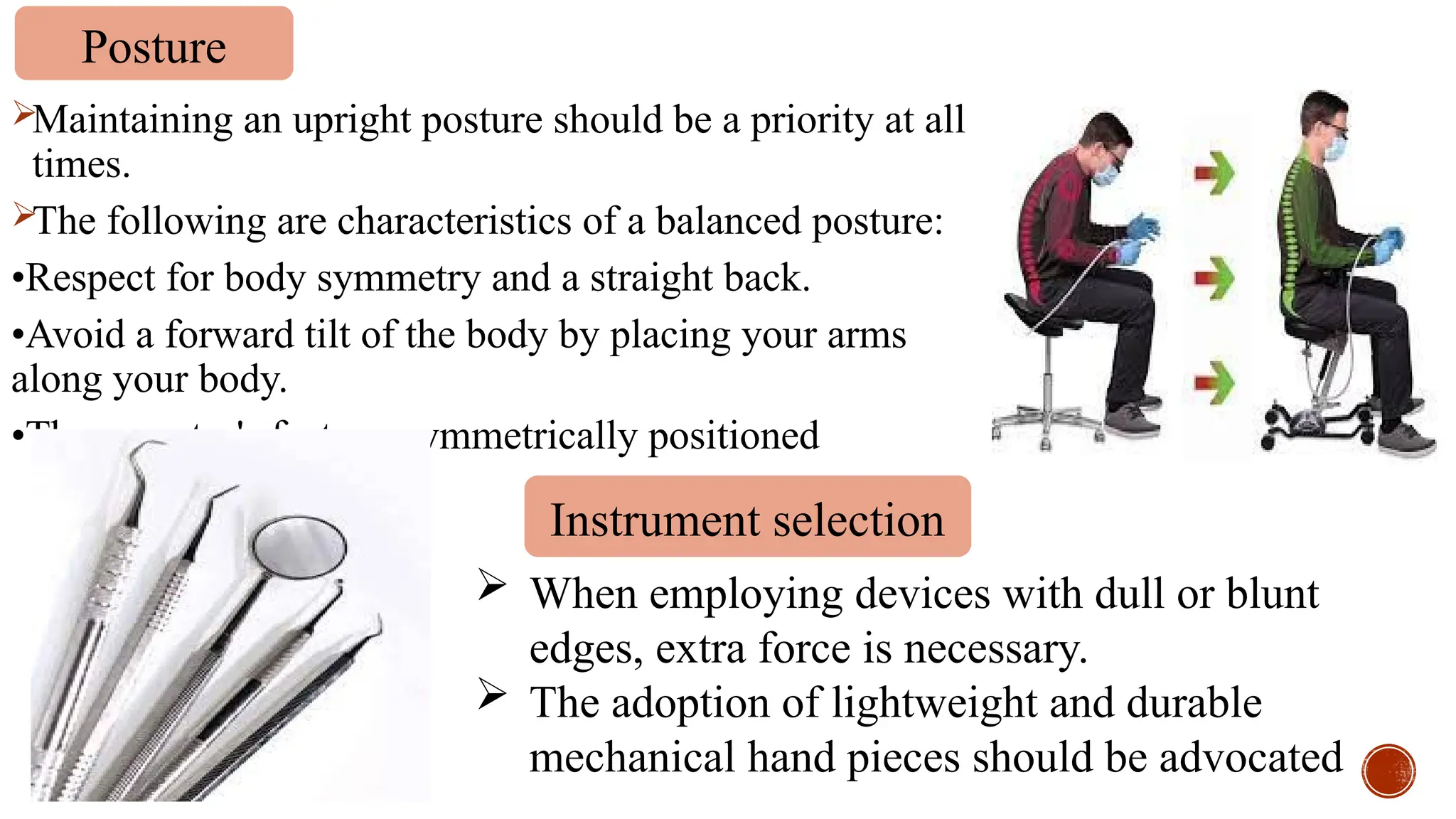
The document discusses the importance of ergonomics in dentistry, highlighting how poor ergonomic practices can lead to musculoskeletal disorders (MSDs) in dental professionals. It covers the definition of ergonomics, common injuries, and preventative measures, including tool design and proper workstation setup. Additionally, it emphasizes the benefits of ergonomically designed furniture and instruments to enhance practitioner comfort and reduce the risk of long-term injuries.