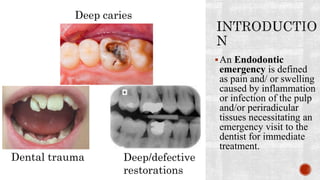
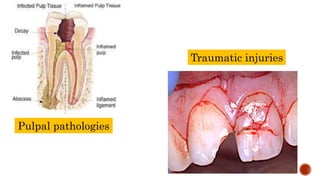
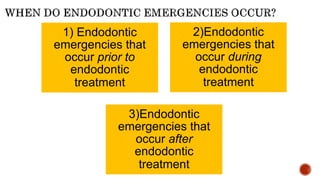
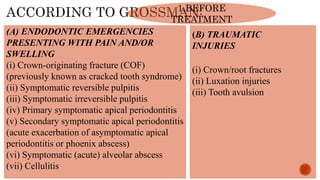
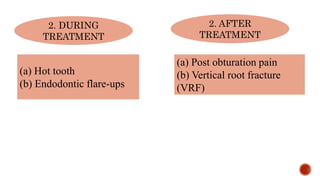
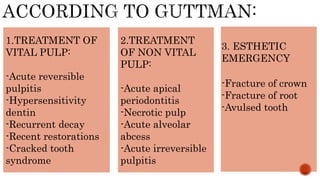
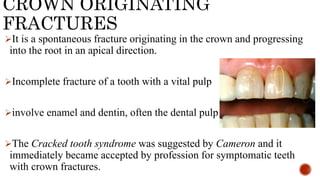
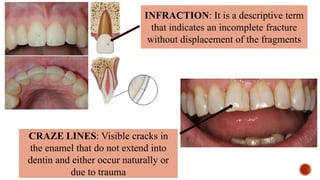
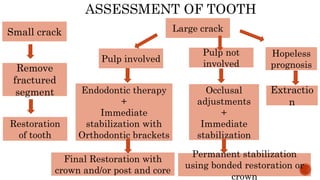
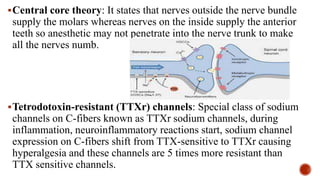
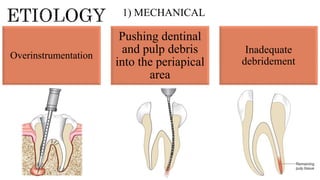
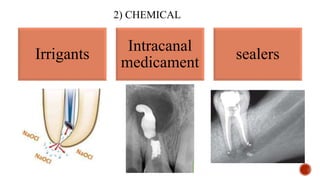
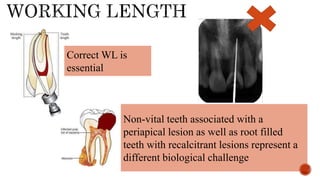
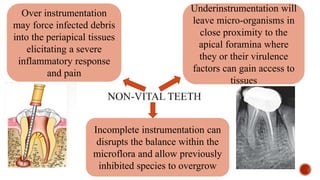
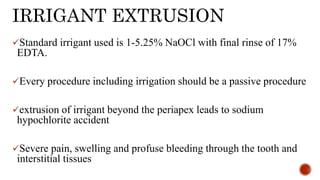
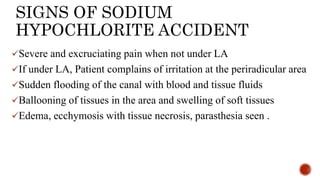
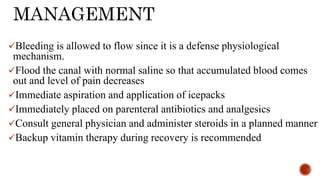
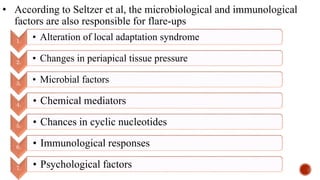
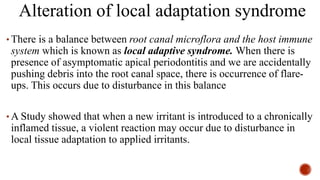
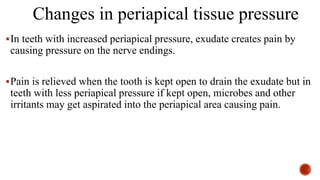
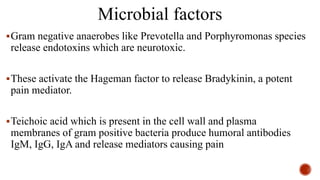
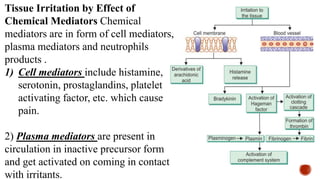
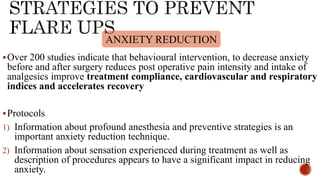
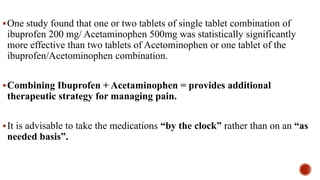
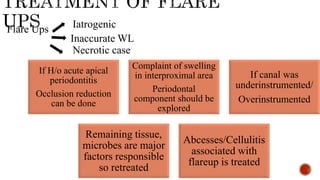
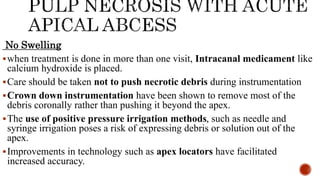
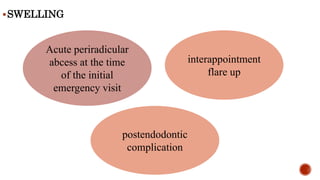
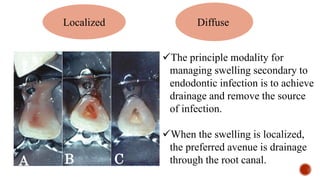
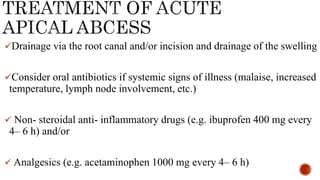
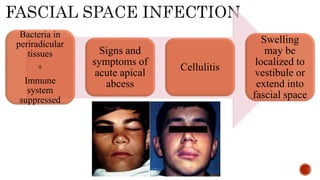
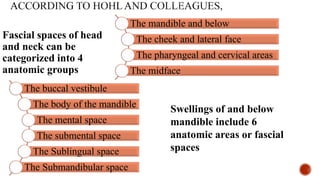
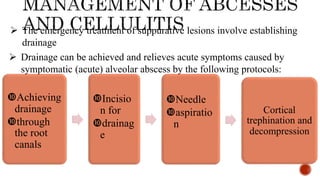
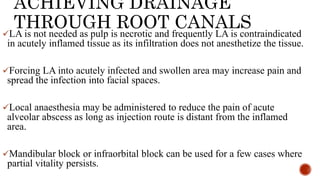
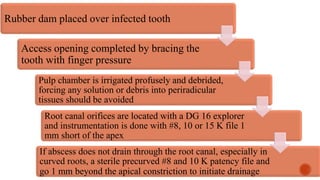
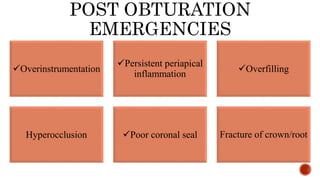
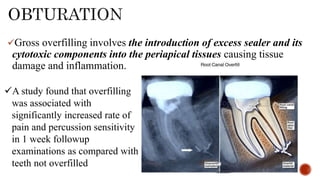
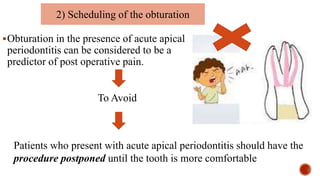
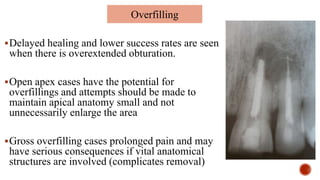
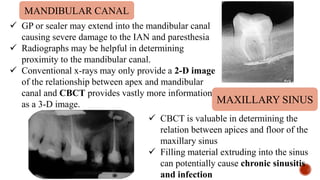
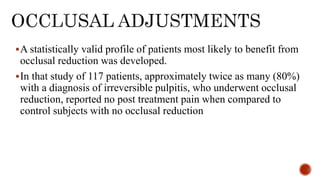
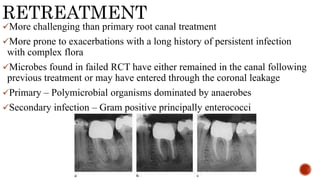
Endodontic emergencies arise from inflammation or infection of the dental pulp and surrounding tissues, necessitating urgent dental care. They can occur before, during, or after treatment and include conditions like reversible/irreversible pulpitis and traumatic injuries. Management strategies include proper diagnosis, effective use of local anesthesia, and careful treatment to prevent complications such as flare-ups or periapical issues.