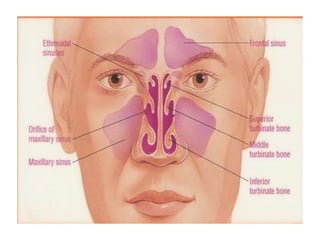
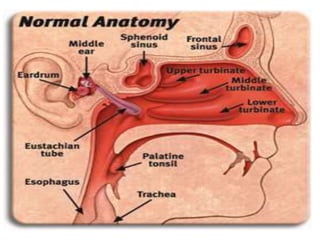
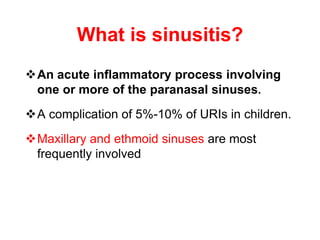
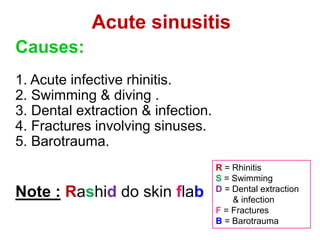
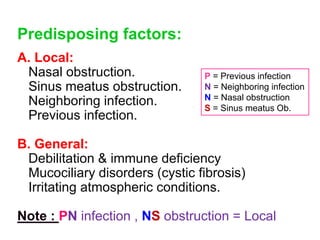
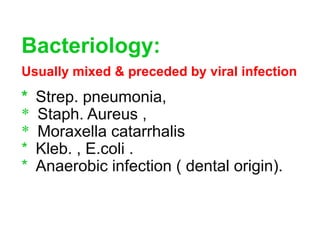
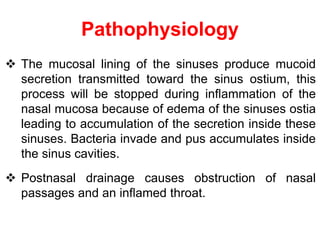
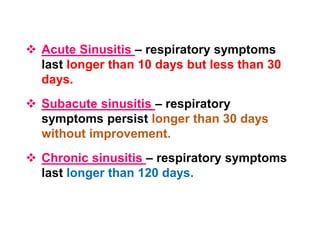
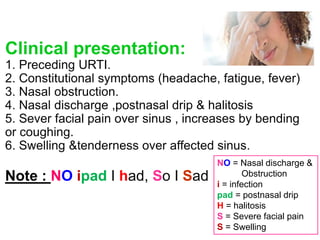
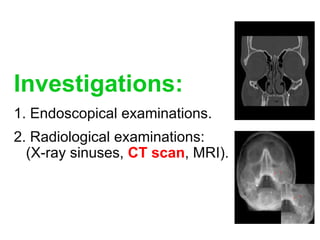
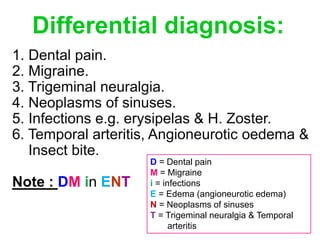
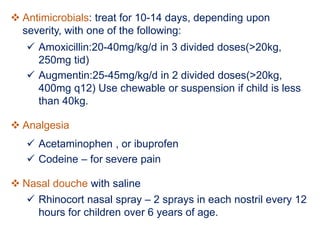
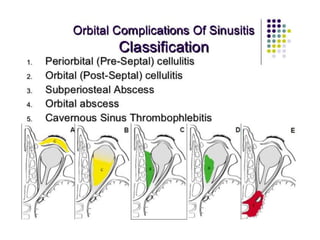
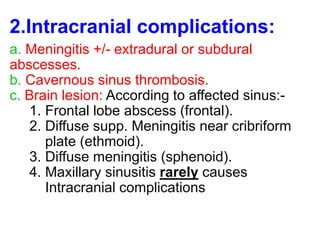
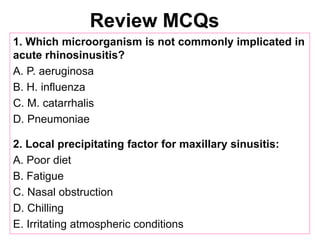
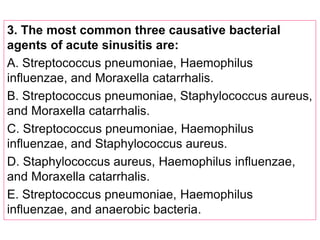
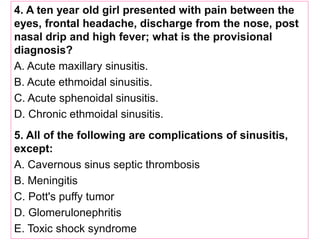
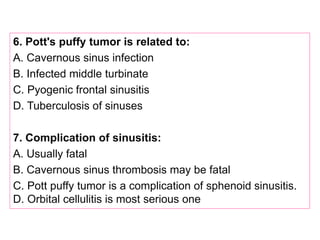
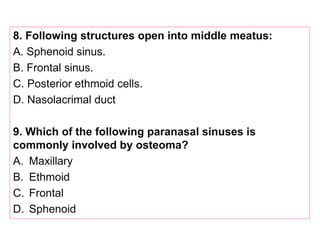
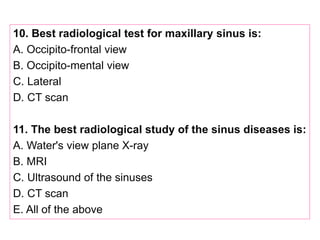
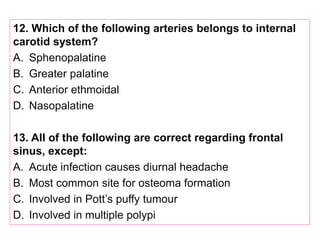
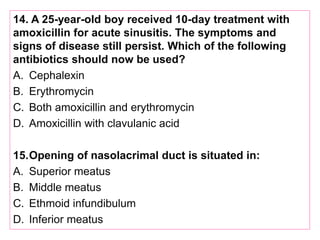
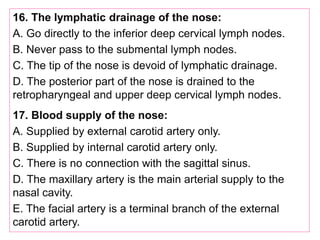
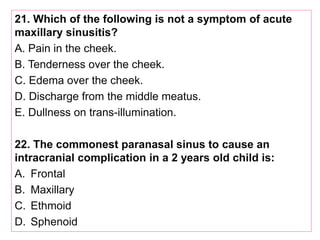
This document discusses sinusitis, beginning with a definition and causes. It then covers the clinical presentation, investigations, differential diagnosis, treatment, and complications of both acute and chronic sinusitis. Key points include that acute sinusitis is usually preceded by a viral upper respiratory infection and is commonly caused by Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. Facial pain, nasal discharge, and swelling over the affected sinus are common symptoms. Treatment involves antibiotics, analgesics, nasal decongestants, and irrigation. Complications can include orbital or intracranial infections if not properly treated.