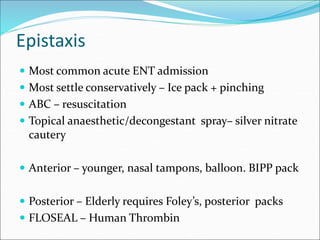
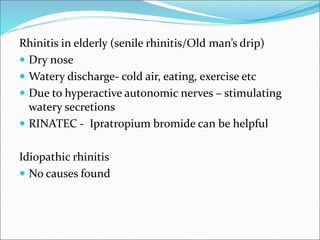
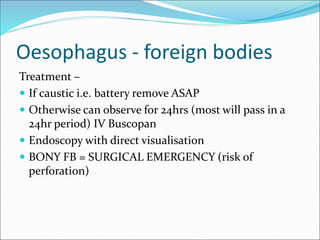
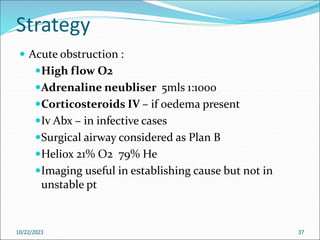
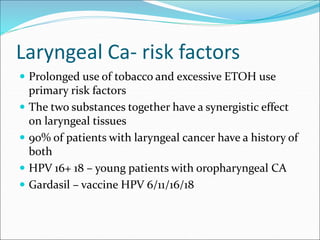
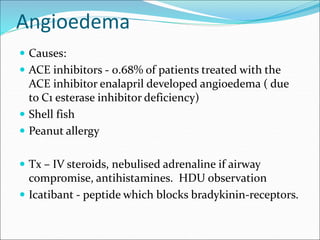
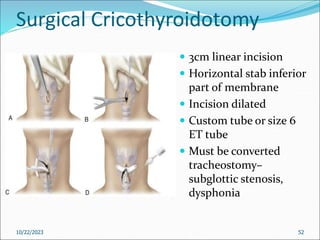
This document provides an overview of common acute ENT conditions that may be encountered in a casualty setting. It discusses tonsillitis, epistaxis, rhinitis, sinusitis, laryngeal cancer risk factors, angioedema, and foreign body obstruction of the esophagus and airway. Management strategies are outlined for each condition. It emphasizes the importance of early discussion with ENT specialists for any cases involving airway obstruction or stridor. Surgical cricothyroidotomy and tracheotomy are described as emergency procedures to secure the airway if needed.