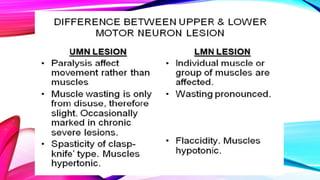
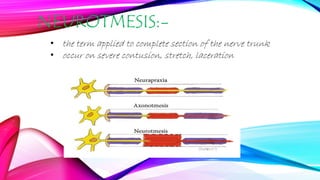
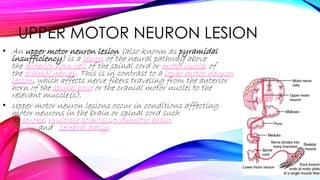
This document discusses changes in electrical reactions that occur with diseases or injuries of motor nerves or muscles. It describes different types of lesions that can occur at the neuron, nerve, neuromuscular junction, and muscle levels. Specifically, it details upper motor neuron lesions, lower motor neuron lesions, and classifications of nerve injuries. Tests used to analyze electrical reactions include electromyography, nerve conduction velocity tests, and others. Electromyography detects electrical potentials in muscles during contraction and is used to diagnose neuropathies and monitor nerve and muscle recovery from injury.



![LOWER MOTOR NEURON
LESION
• A lower motor neuron lesion is a lesion which affects nerve
fibers traveling from the anterior grey column of the spinal
cord to the relevant muscle(s) – the lower motor neuron.[1]
• One major characteristic used to identify a lower motor
neuron lesion is flaccid paralysis – paralysis accompanied
by loss of muscle tone. This is in contrast to an upper motor
neuron lesion, which often presents with spastic paralysis –
paralysis accompanied by severe hypertonia.](https://image.slidesharecdn.com/electricalreaction-150510063157-lva1-app6892/85/Electrical-reaction-6-320.jpg)