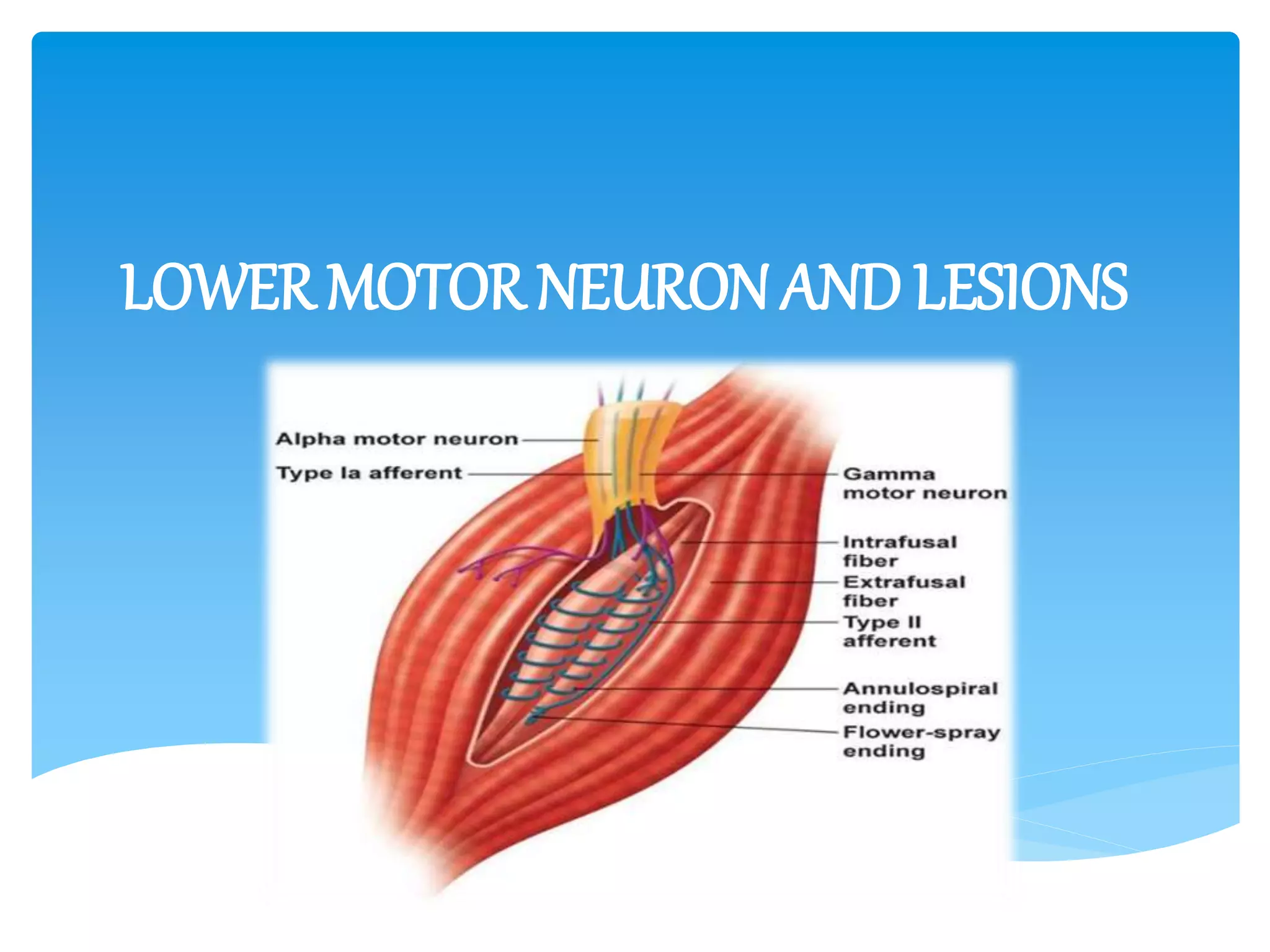
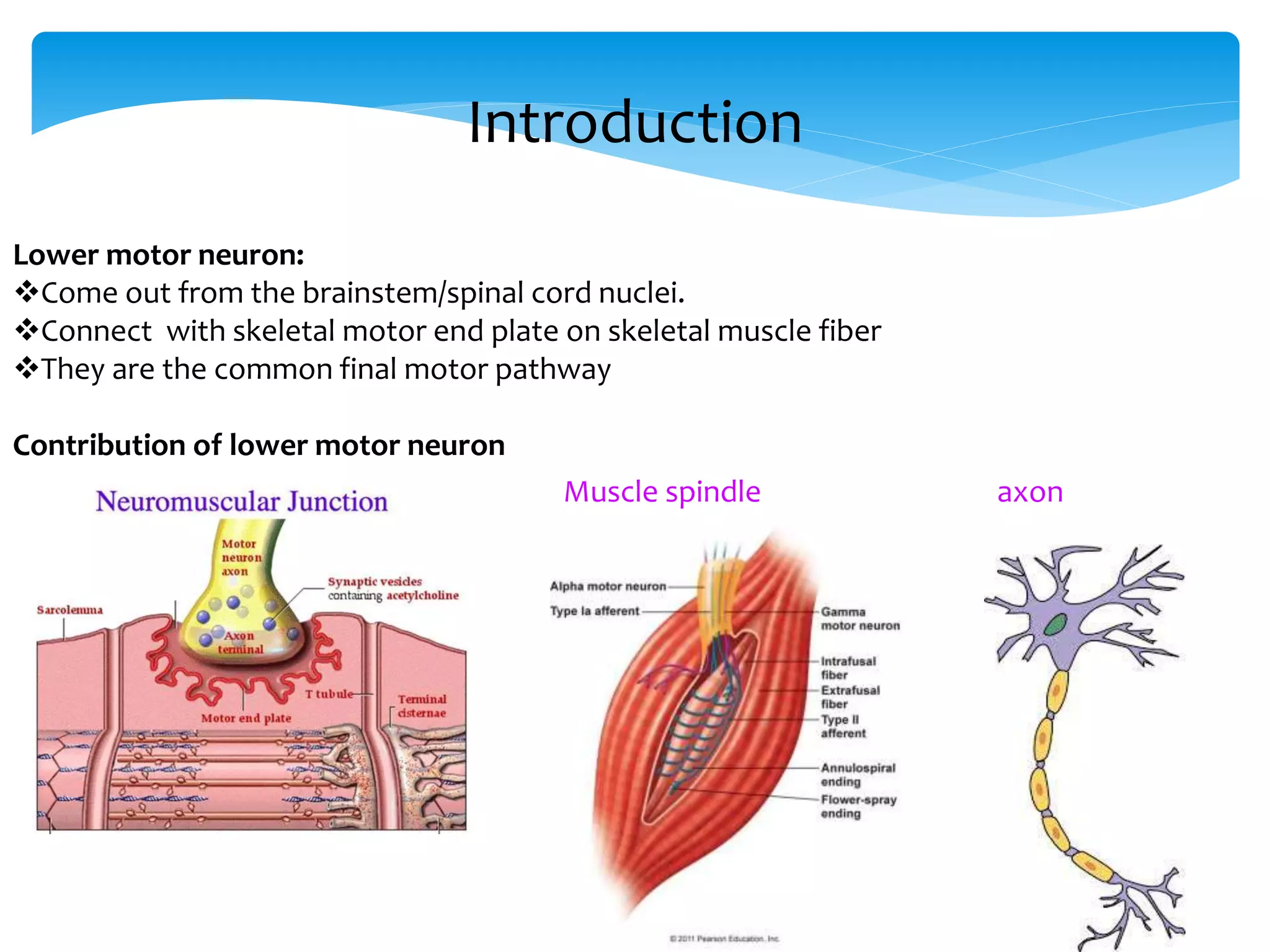
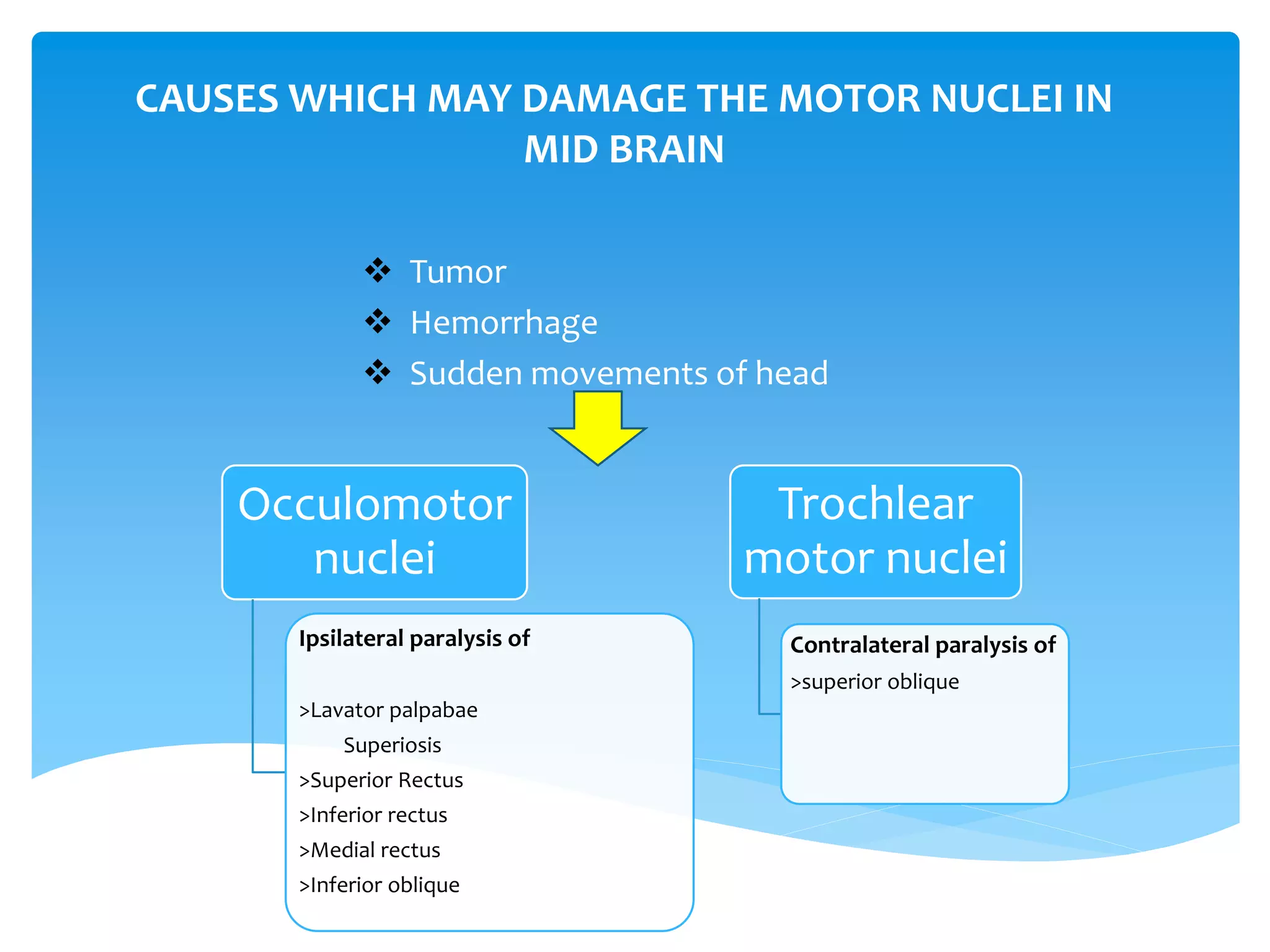
Lower motor neuron lesions can occur in the nuclei, cranial nerves, spinal nerves, axons, muscles, or motor end plates. Damage to motor nuclei in the midbrain can cause paralysis of specific eye muscles. Injuries in the pons can weaken facial or eye muscles. In the medulla, motor nuclei injuries can affect tongue, jaw, or eye muscles. Axon injuries include neurapraxia, axonotmesis, and neurotmesis. Denervated muscles undergo reaction of degeneration and loss of reflexes. Lower motor neuron lesions cause flaccid paralysis, muscle atrophy, fasciculations, and contractures.