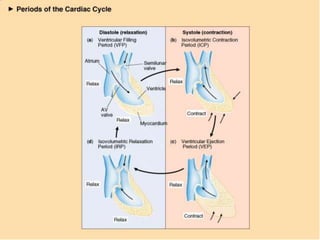
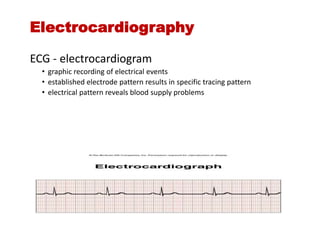
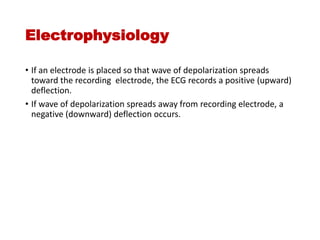
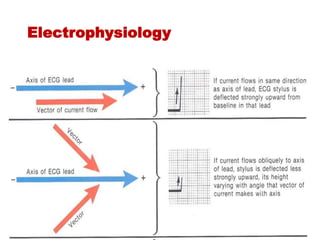
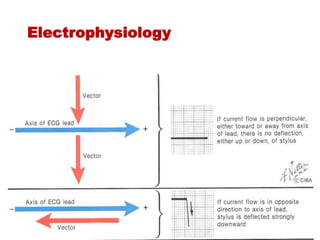
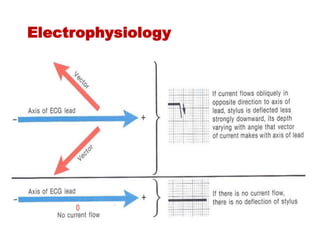
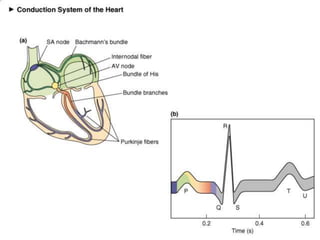
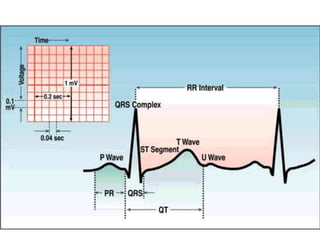
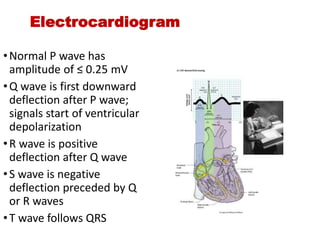
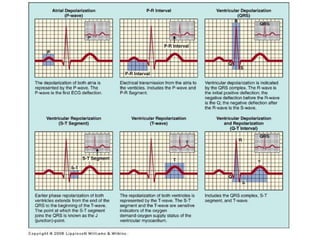
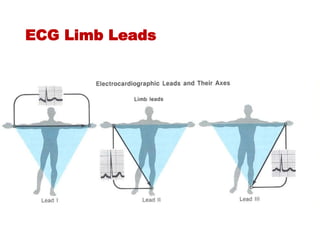
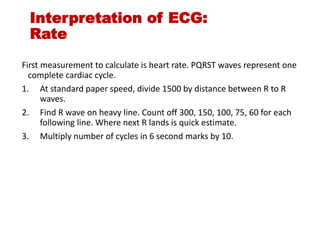
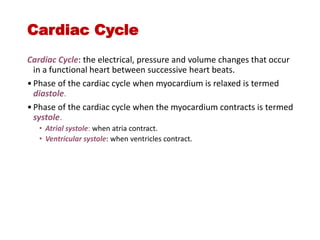
The document discusses the electrocardiogram (ECG or EKG), which records the electrical activity of the heart. It describes the cardiac cycle, including the electrical and mechanical events that occur with each heartbeat. Specifically, it discusses the phases of atrial systole and ventricular systole, as well as the mechanical events of ventricular filling, isovolumetric contraction, ventricular ejection, and isovolumetric relaxation. It also explains how electrical changes in heart tissue cause mechanical changes like muscle contraction.

![Mechanical Events of the
Cardiac Cycle
1. Ventricular Filling Period [ventricular diastole,
atrial systole]
2. Isovolumetric Contraction Period [ventricular
systole]
3. Ventricular Ejection Period [ventricular
systole]
4. Isovolumetric Relaxation Period [ventricular
diastole, atrial diastole]](https://image.slidesharecdn.com/ecgcompletelecture-240204125716-3aff92d9/85/ECG-complete-lecture-notes-along-with-interpretation-3-320.jpg)