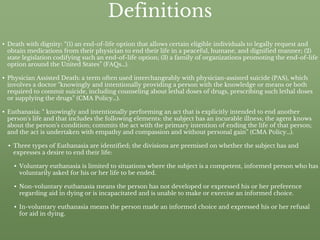
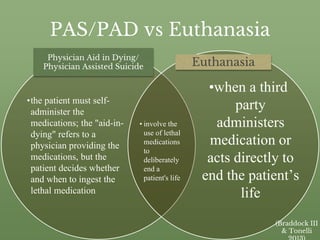
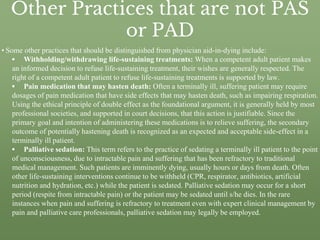
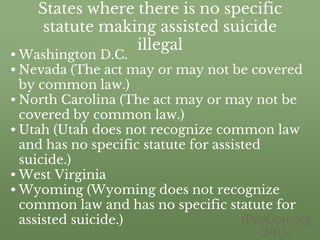
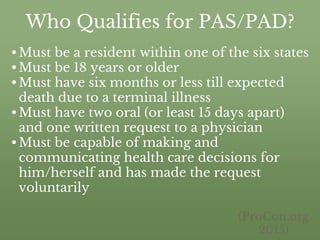
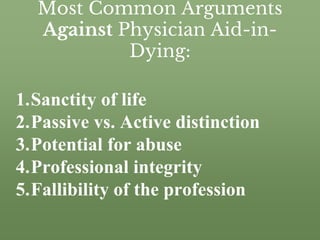
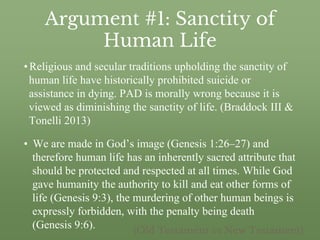
This document discusses physician aid in dying and definitions of related terms like death with dignity, physician assisted suicide, and euthanasia. It outlines where physician aid in dying is currently legal and the eligibility requirements. The document also presents some of the most common arguments against physician aid in dying, including concerns about the sanctity of life, distinguishing between passive and active actions, and potential for abuse. It then provides counter arguments for each of these common positions against physician aid in dying.