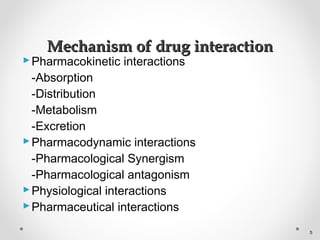
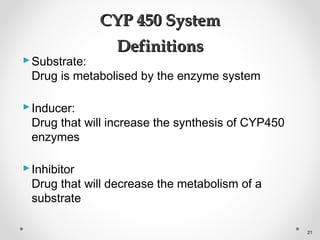
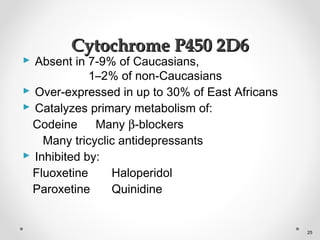
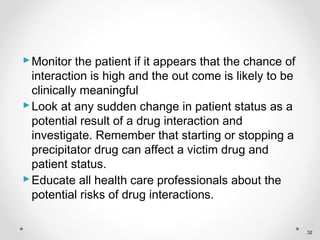
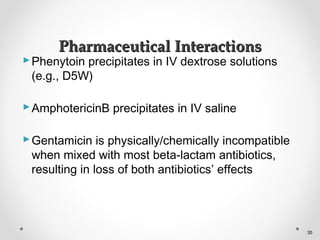
Drug interactions can occur when one drug alters the effects of another drug. They can be either harmful or beneficial. Common causes of interactions include one drug inhibiting or inducing the metabolic pathways of another drug. This can increase or decrease drug levels in the body, potentially causing toxic effects or reducing therapeutic effectiveness. It is important for pharmacists and clinicians to be aware of potential drug interactions and monitor patients taking multiple medications.