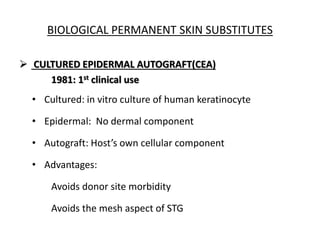
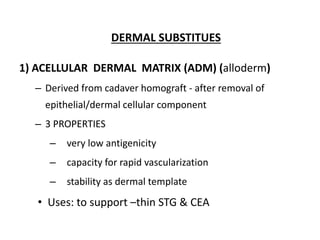
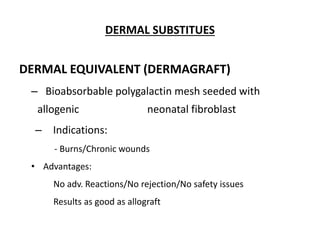
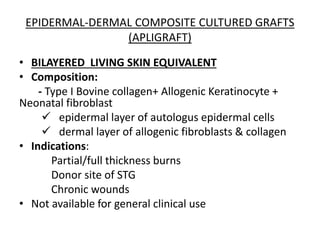
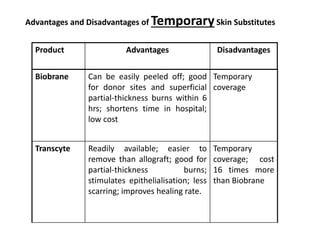
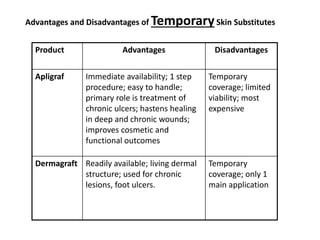
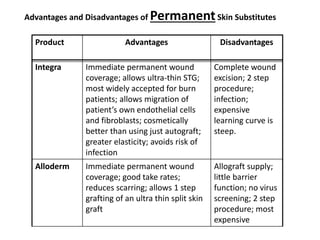
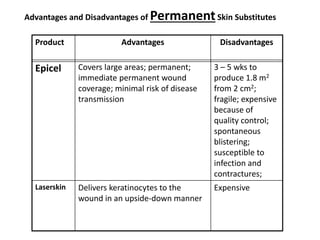
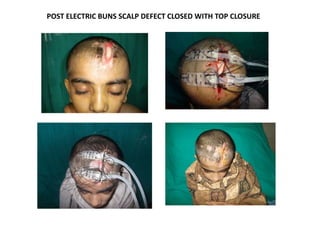
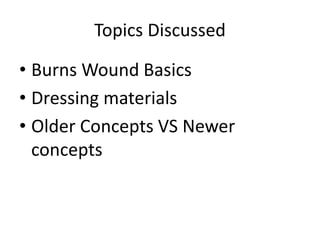
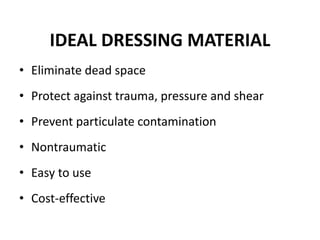
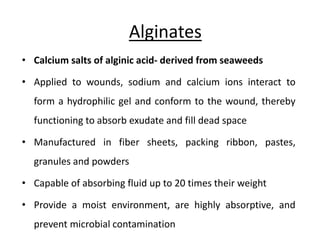
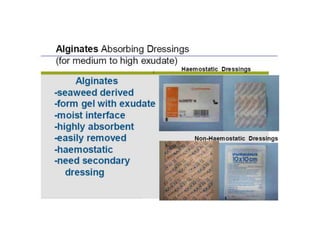
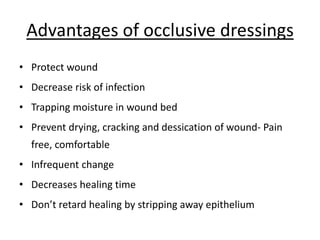
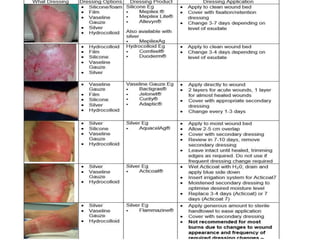
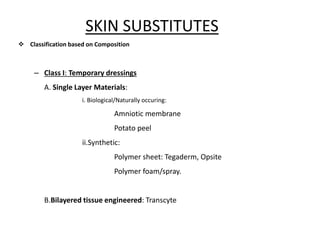
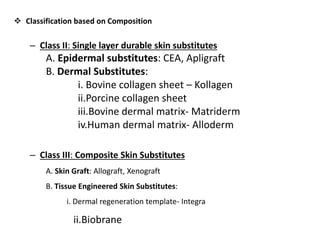
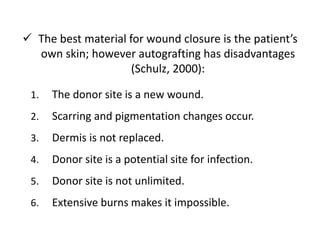
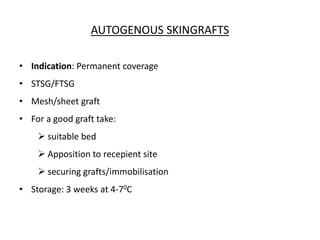
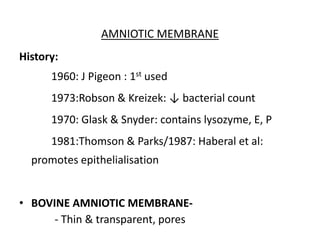
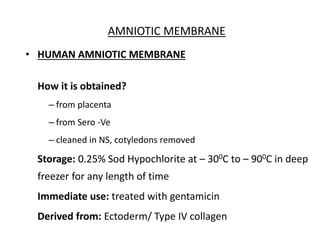
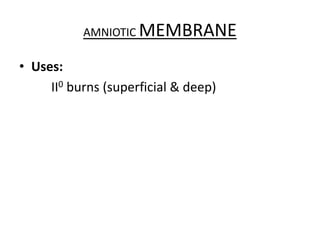
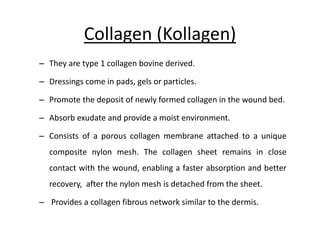
The document outlines the principles and materials used for dressing burns, emphasizing the importance of maintaining a moist environment while preventing infection and fluid loss. It categorizes dressing types into conventional and synthetic occlusive categories, detailing their properties, applications, and limitations. Additionally, it discusses biological coverings, skin substitutes, and the advantages and disadvantages of various dressing techniques for effective wound management.









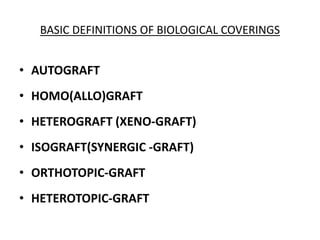
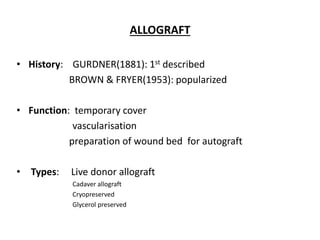
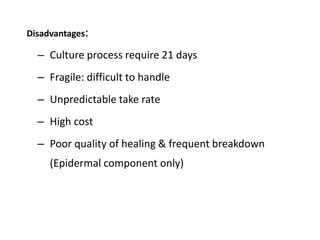
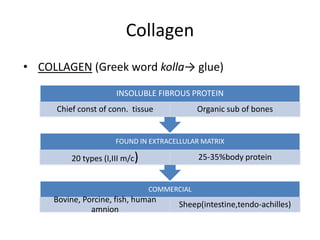
![• Disease transmission : Bacterial, HIV,CMV (discard if
pathogenic bacteria/fungi are present[AATB])
• Rejection: Contains Langerhans cells(Class II HLA)
• Lack of availability
ALLOGRAFT
Disadvantages:-](https://image.slidesharecdn.com/dressingmaterialsinburns-171201153511/85/Dressing-materials-in-burns-69-320.jpg)





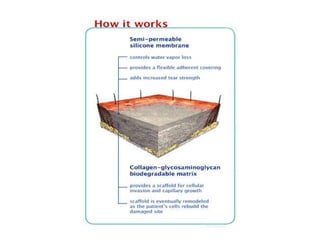
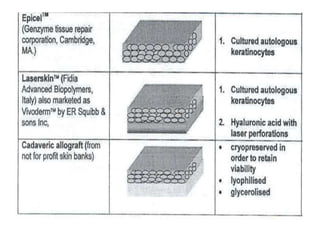
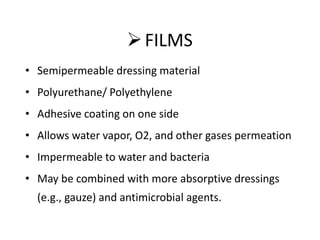
![(INTEGRA)
[Burkes & Yannas Artificial skin]
inner biodegradable memb.
[bovine collagen+
chondroitin SO4]
(dermal component)
Gets vascularised,
Fibroblasts migrate
Outer silicone(100μm)
[temporary]
(epiderm. component)
Protects wound from
dessication/infection
Removed after 3 wks](https://image.slidesharecdn.com/dressingmaterialsinburns-171201153511/85/Dressing-materials-in-burns-92-320.jpg)