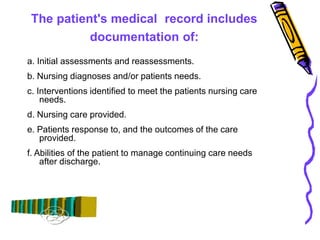
This document provides guidelines and definitions for nursing documentation. It discusses how documentation includes interactions between health professionals and patients, administered tests and treatments, and patient responses. The patient's medical record contains initial assessments, nursing diagnoses, care plans, provided care, patient outcomes, and discharge abilities. Nursing documentation is part of the clinical record written by nurses regarding a patient's health status, needs, care, and response. Documentation supports that care was given, allows communication, provides legal protection, and supports reimbursement, quality assurance, education, and research. Medical records contain identifying information, diagnoses, health history, treatment plans, assessments, medications, diet, teaching, test results, and discharge summaries. The document outlines general documentation guidelines regarding formatting,