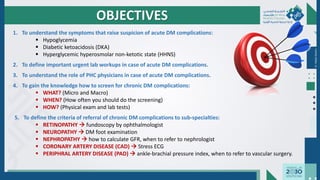
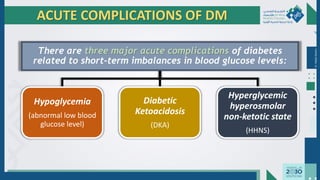
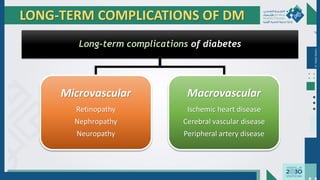
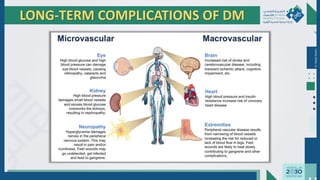
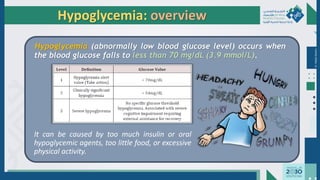
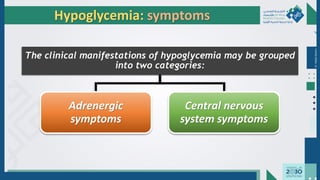
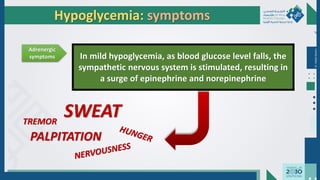
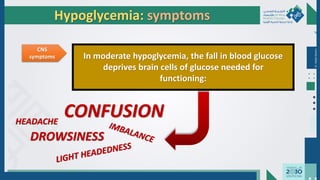
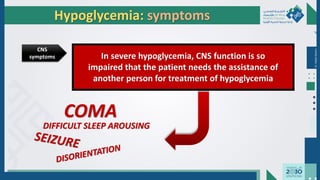
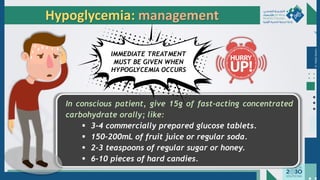
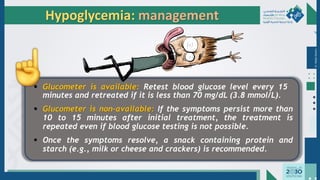
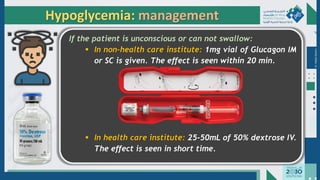
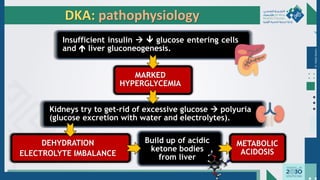
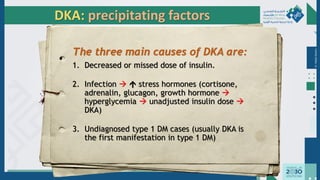
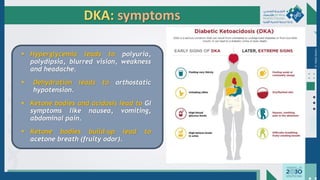
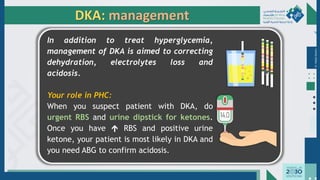
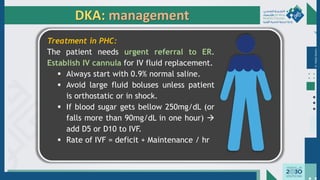
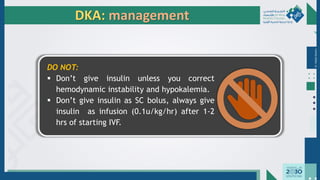
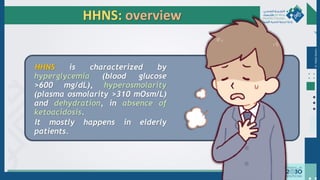
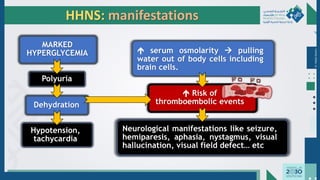
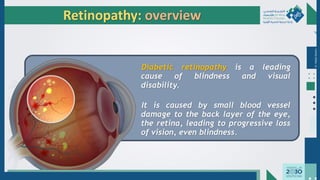
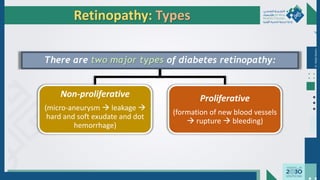
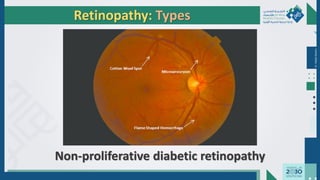
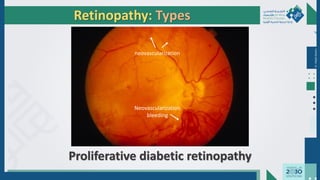
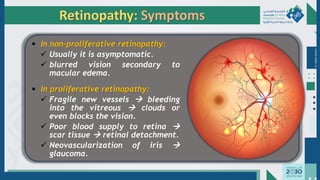
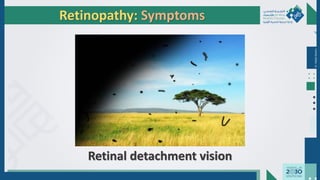
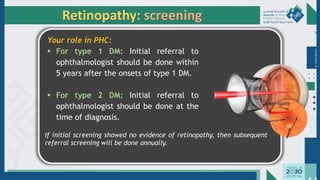
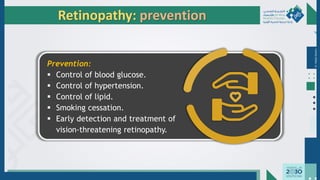
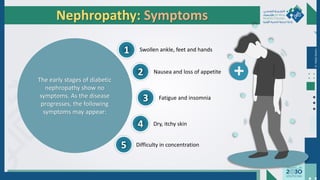
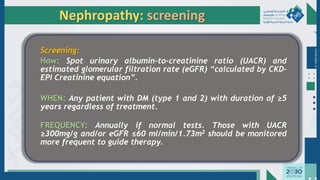
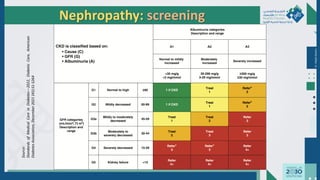
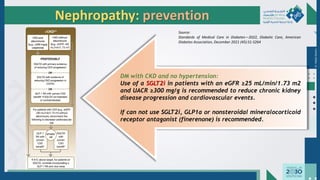
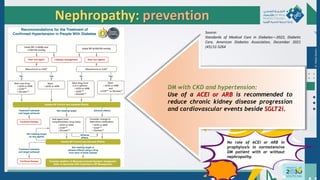
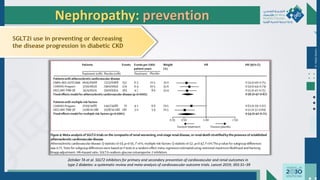
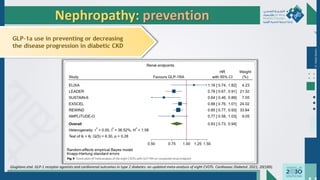
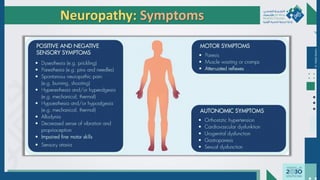
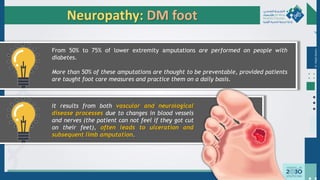
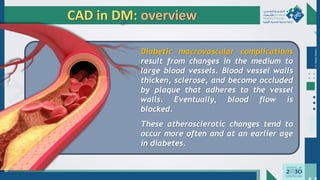
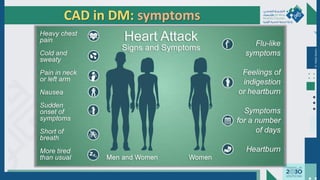
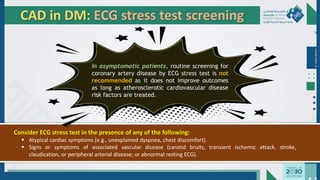
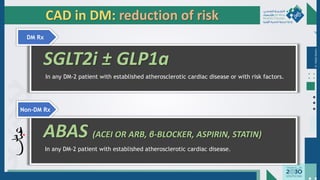
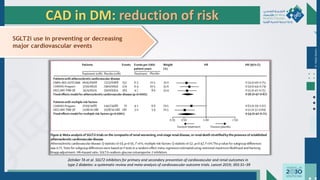
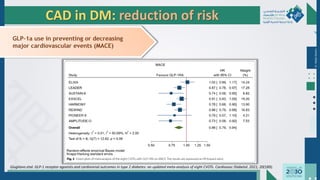
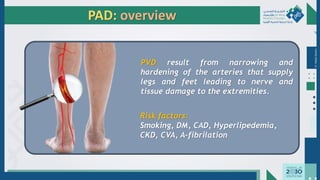
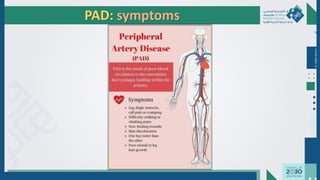
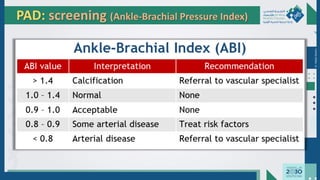
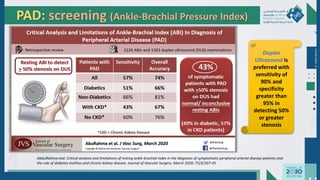
The document outlines the acute and long-term complications of diabetes mellitus, highlighting symptoms, urgent lab workups, and the role of primary healthcare physicians in managing these conditions. Key acute complications include hypoglycemia, diabetic ketoacidosis (DKA), and hyperglycemic hyperosmolar non-ketotic state (HHNS), while long-term complications encompass microvascular and macrovascular issues such as retinopathy, nephropathy, and coronary artery disease. It emphasizes the importance of screening, early detection, and proper management to prevent severe outcomes and enhance patient care.