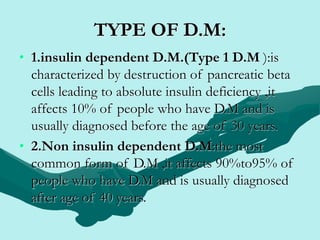
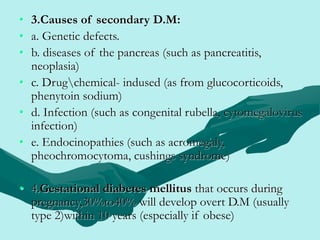
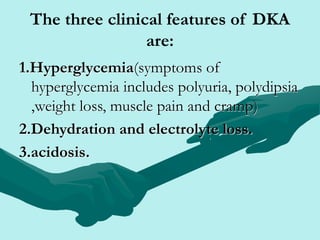
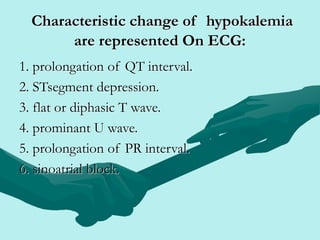
This document outlines the key points about diabetes mellitus and its acute complications. It begins with definitions of diabetes mellitus and an overview of the different types. The acute complications discussed are diabetic ketoacidosis (DKA), hyperglycemic hyperosmolar nonketotic syndrome (HHNS), and hypoglycemia. For DKA, it covers causes, pathophysiology, signs/symptoms, diagnostic tests, medical management including fluid resuscitation and insulin therapy, and nursing care. HHNS is defined as a hyperglycemic condition without acidosis seen in older patients. Risk factors, signs, and treatment are also summarized.