Disorders of protein metabolism were presented. Key points included:
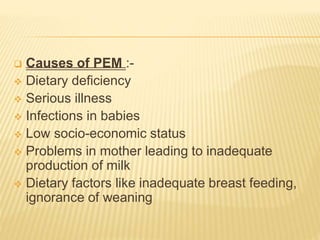
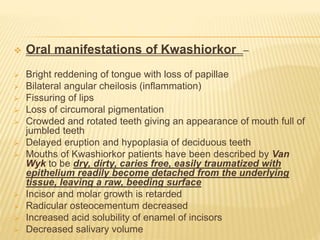
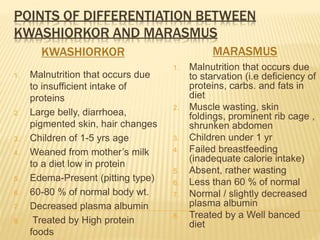
- Protein energy malnutrition (PEM) was discussed, including kwashiorkor caused by insufficient protein intake and marasmus caused by total starvation. Symptoms and treatments were described.
- Amyloidosis is caused by misfolded proteins depositing in tissues. It was classified and systemic, hereditary, and localized forms were outlined. Oral manifestations can include enlarged tongue or palatal nodules. Diagnosis involves biopsy and Congo red staining.
- Gout is caused by uric acid crystal deposition in joints due to diminished renal excretion or increased intake of purines. It commonly affects men and risk increases with age and weight. Sympt