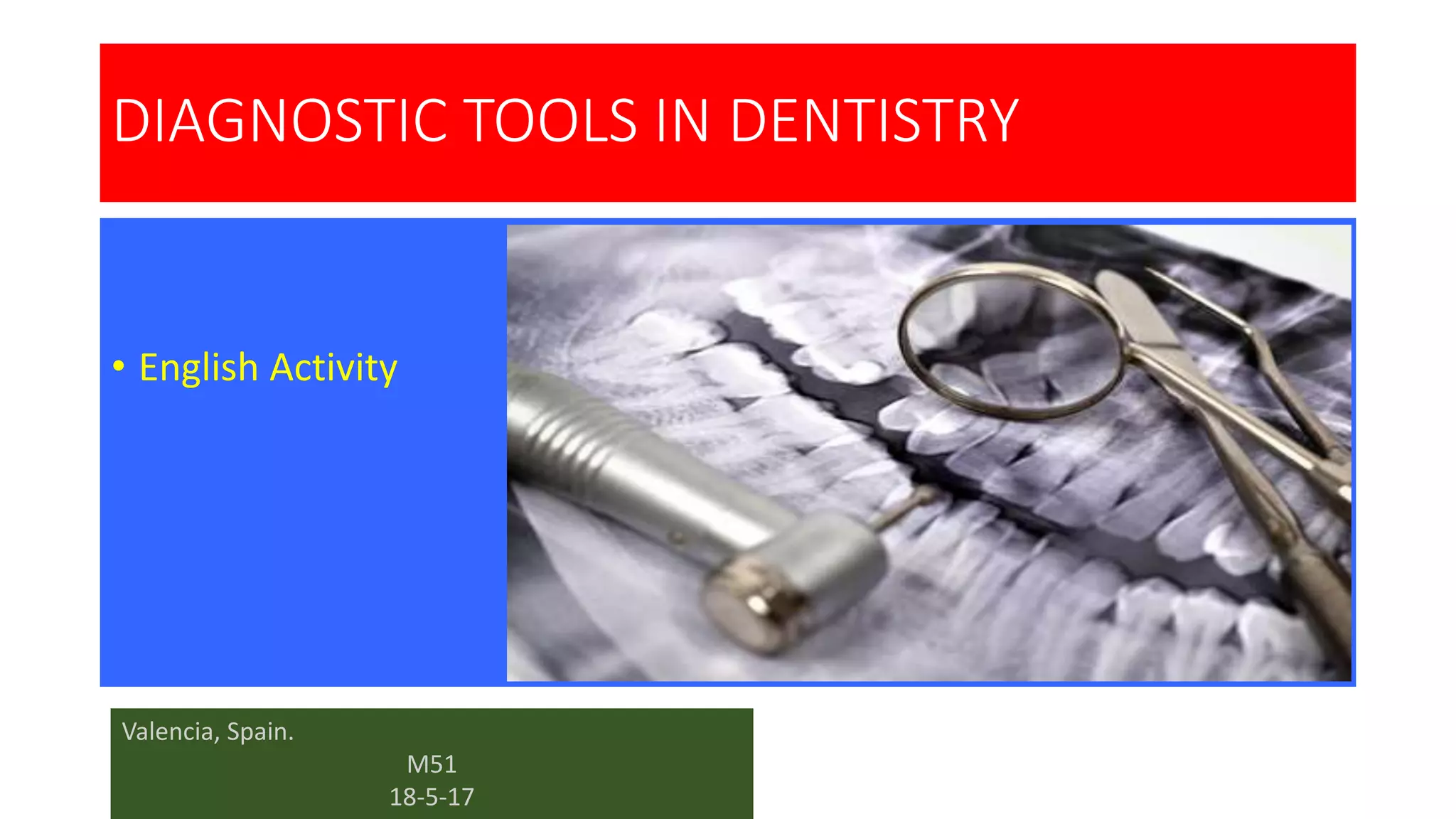
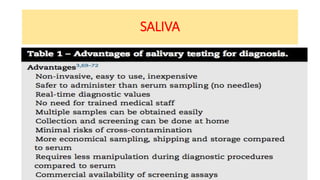
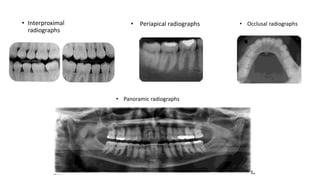
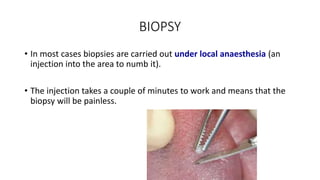
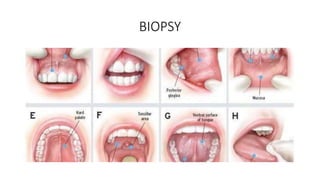
The document discusses various diagnostic tools in dentistry, focusing on saliva tests, x-rays, and biopsies for diagnosing oral and systemic diseases. Saliva is highlighted for its potential in early diagnosis of conditions such as cardiovascular disease, HIV/AIDS, and oral cancer. Additionally, it covers x-ray techniques and the importance of biopsies in determining the presence of diseases, emphasizing the need for proper diagnostic practices in dental healthcare.