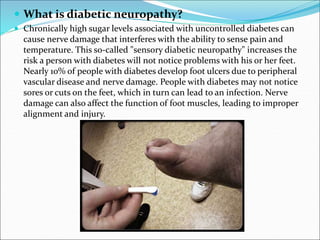
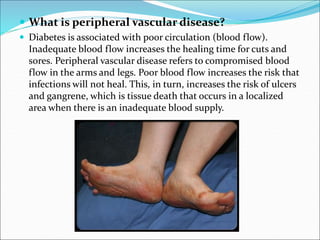
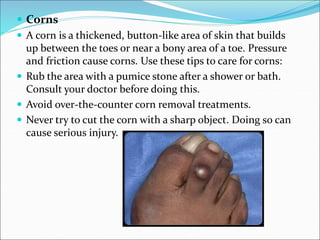
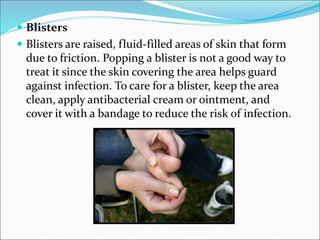
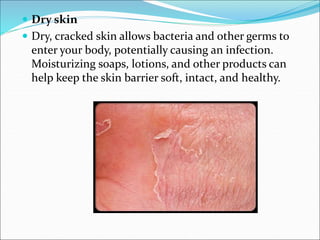
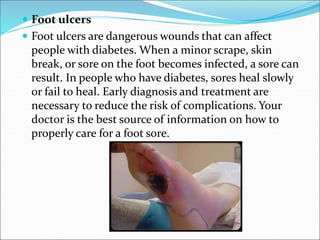
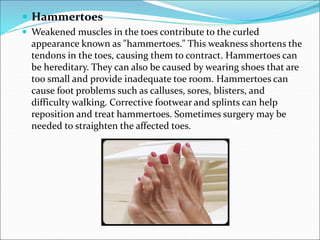
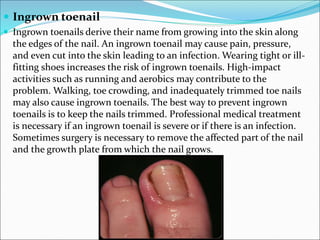
Diabetes can lead to serious foot complications, primarily through diabetic neuropathy and peripheral vascular disease, affecting nerve function and blood flow in the feet. Common issues include foot ulcers, fungal infections, calluses, corns, blisters, and ingrown toenails, all of which can worsen if not properly managed. Preventive care is crucial, including daily foot inspections, proper hygiene, appropriate footwear, and regular check-ups with a podiatrist to avoid serious complications.