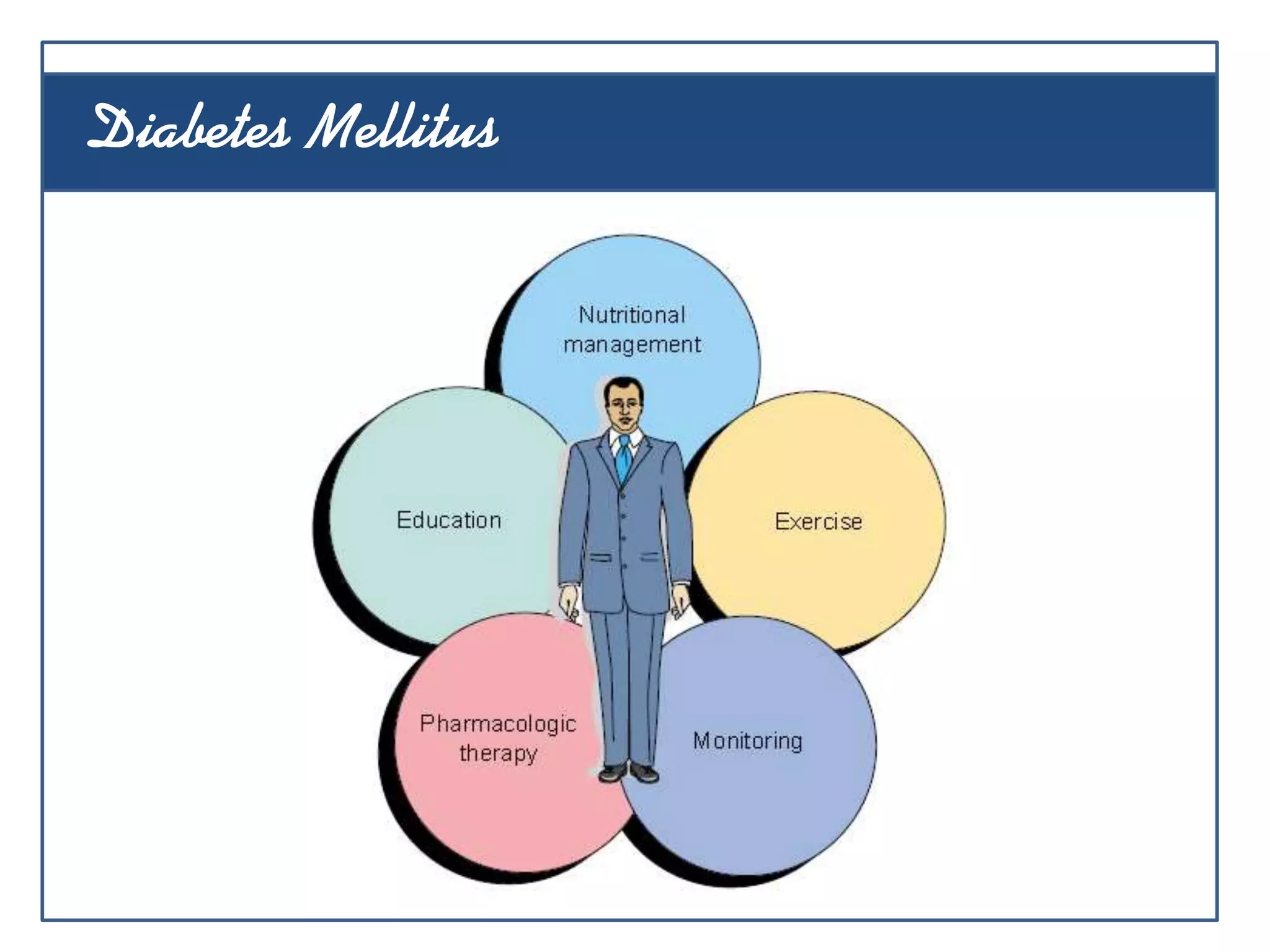
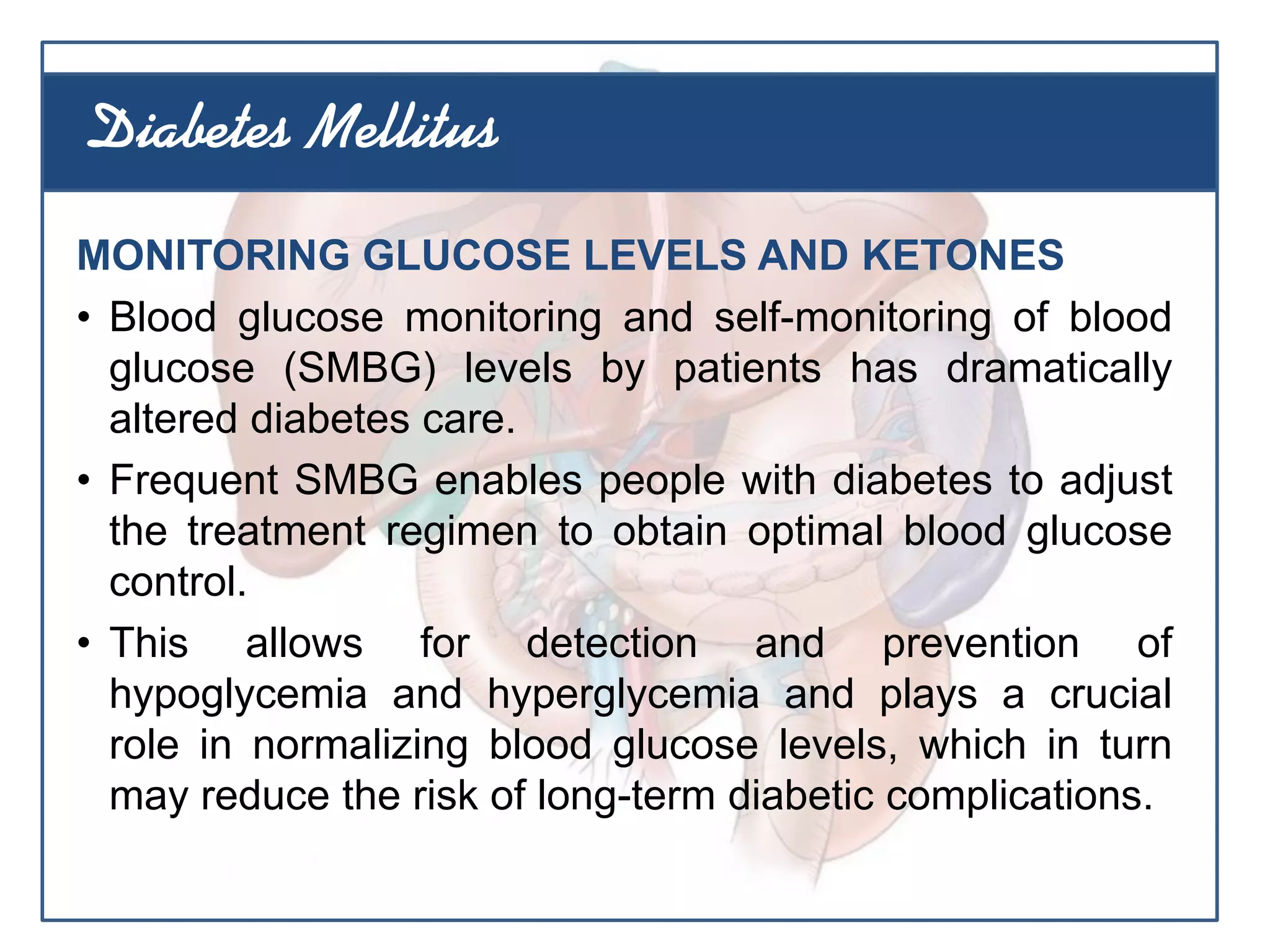
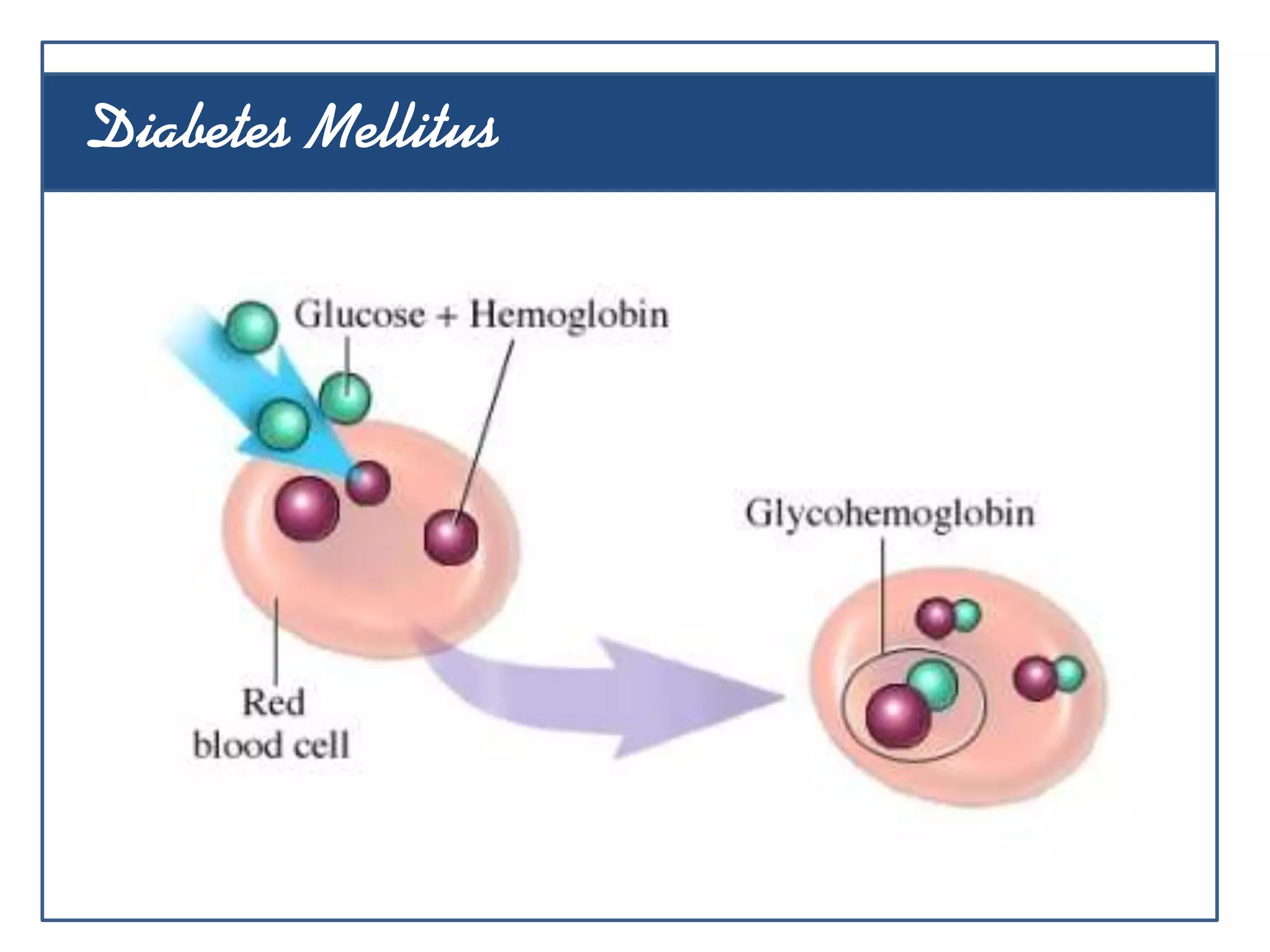
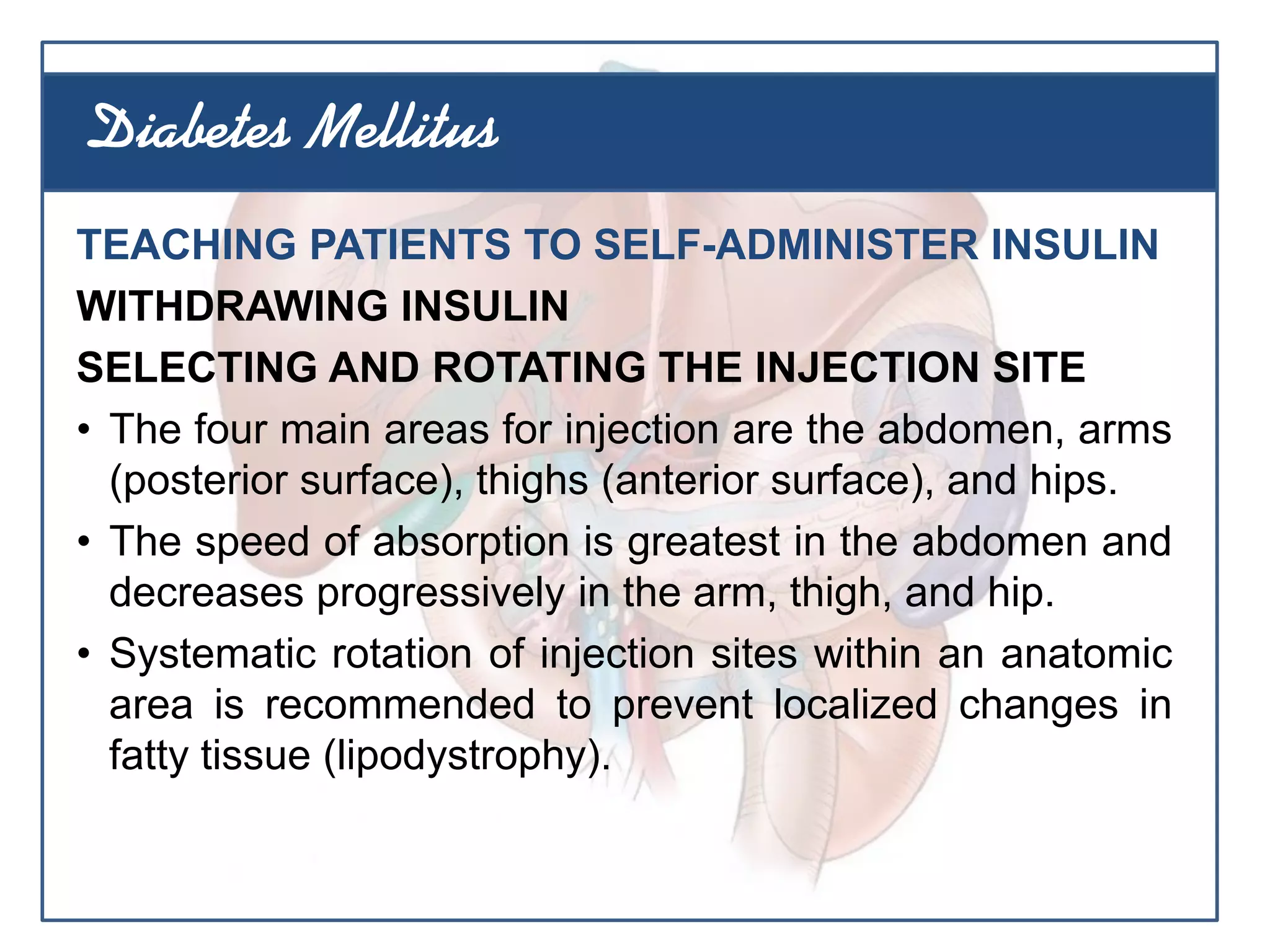
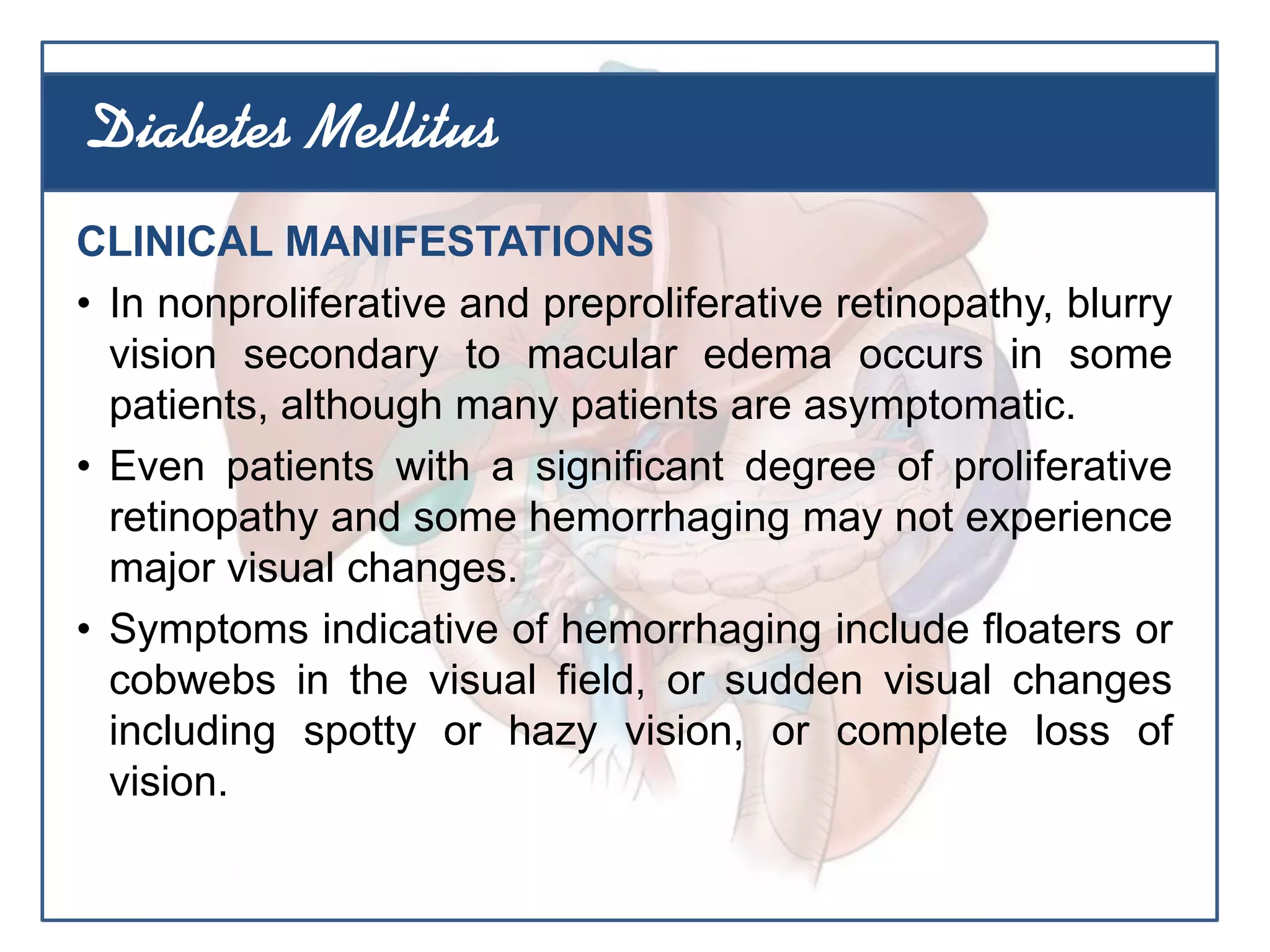
This document outlines 13 learning objectives for a lecture on diabetes mellitus. The objectives cover differentiating between type 1 and type 2 diabetes, describing risk factors and clinical manifestations, explaining diagnostic tests and management strategies, and identifying complications and their prevention. The lecture content will define diabetes, classify its types, discuss pathophysiology, and describe nutritional, exercise, monitoring, pharmacological, and educational approaches to management.

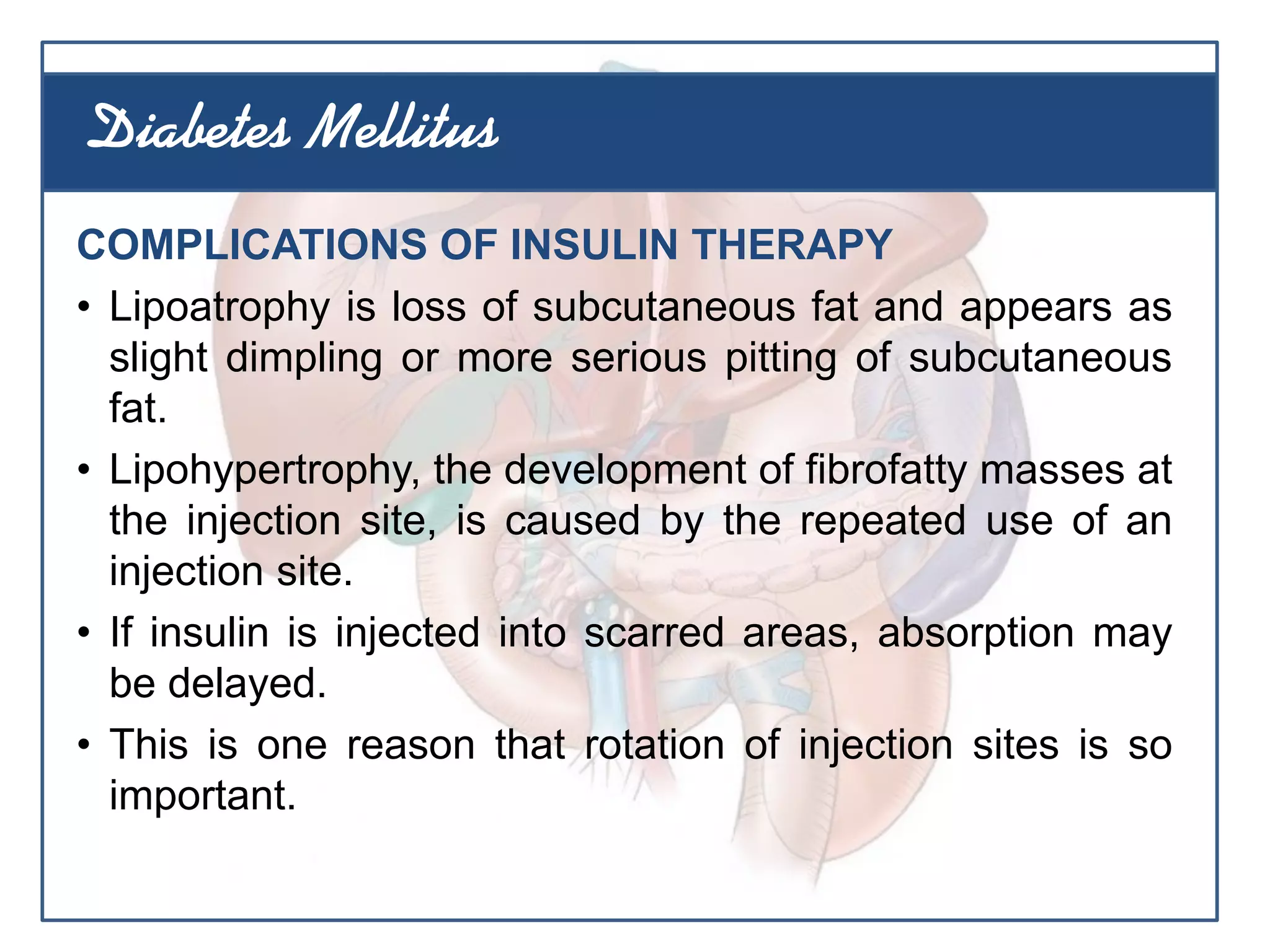




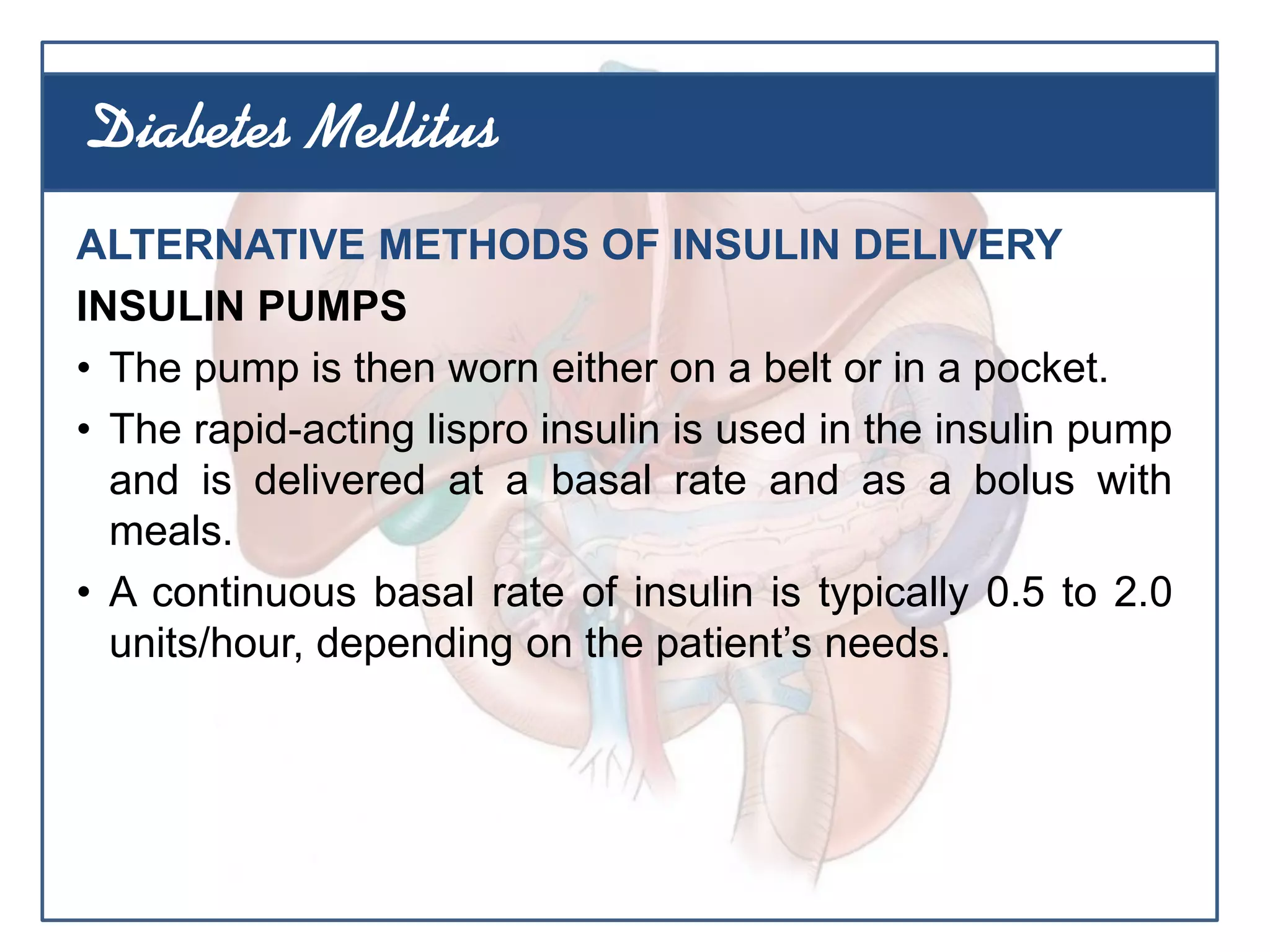
![MEDICAL MANAGEMENT
• Control of hypertension (the use of angiotensin-
converting enzyme [ACE] inhibitors, such as captopril,
because control of hypertension may also decrease or
delay the onset of early proteinuria)
• Prevention or vigorous treatment of urinary tract
infections
• Avoidance of nephrotoxic substances
• Adjustment of medications as renal function changes
• Low-sodium diet
• Low-protein diet
Diabetes Mellitus](https://image.slidesharecdn.com/diabeteslec-130610050634-phpapp02/75/Diabetes-Lecture-132-2048.jpg)