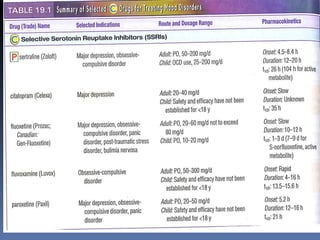
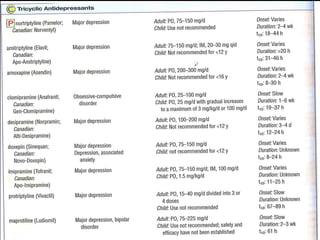
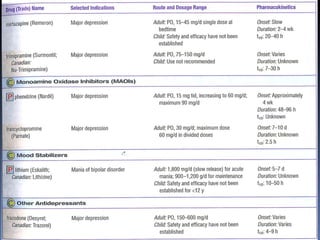
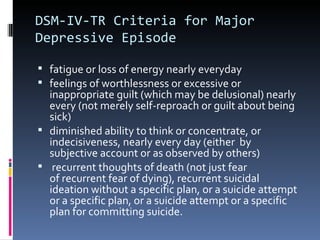
This document discusses mood disorders, specifically depression. It provides the DSM-IV criteria for a major depressive episode, including symptoms such as depressed mood, diminished interest, changes in appetite, insomnia, fatigue, feelings of worthlessness, difficulty concentrating, and suicidal thoughts. It also discusses treatment options, focusing on pharmacotherapy. SSRIs are considered a first-line treatment and details are provided about specific SSRIs, their mechanisms of action, indications, and precautions. Risk factors for suicide are briefly covered.
![Pregnancy and Postpartum
Depression
Postpartum depression affects a small percentage of
mothers
68 to 100 percent relapse in pregnant patients that
discontinue therapy
Evidence suggests increased rates of special care nursery
admission after delivery for children of mothers on SSRIs
SSRIs are secreted in breast milk; however [plasma]
levels are usually very low in mothers that are breast
feeding.](https://image.slidesharecdn.com/depressionsuicide-120223170018-phpapp01-120620121815-phpapp02/85/Depressionsuicide-120223170018-phpapp01-20-320.jpg)
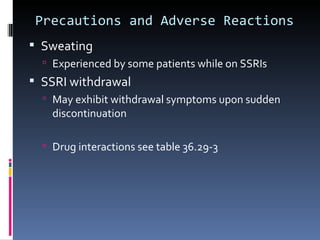
![Precautions and Adverse Reactions
Electrolyte and Glucose Disturbances
SSRIs may decrease [glucose]
Careful monitoring for diabetic patients suggested
Endocrine and Allergic Reactions
SSRIs can decrease prolactin levels
Mammoplasia and galactorrhea in both men and
women
Various types of rashes- 4% of patients
Serotonin syndrome
Concurrent administration of an SSRI with MAOI, L-
Tryptophan or lithium can raise plasma [serotonin]
to toxic levels](https://image.slidesharecdn.com/depressionsuicide-120223170018-phpapp01-120620121815-phpapp02/85/Depressionsuicide-120223170018-phpapp01-26-320.jpg)