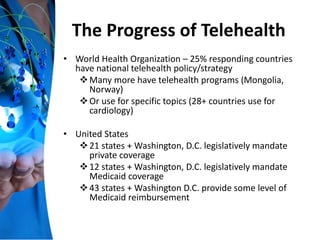
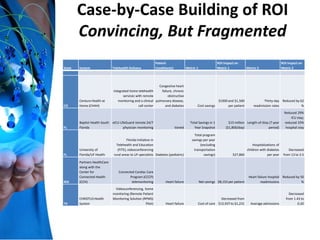
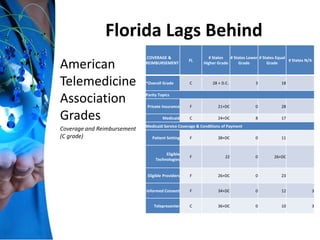
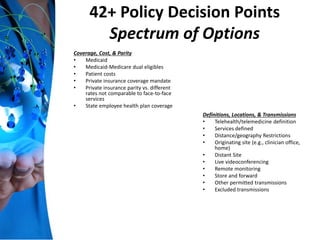
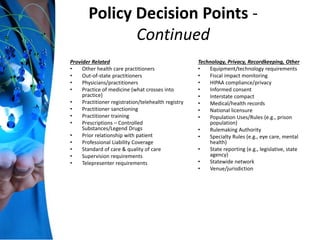
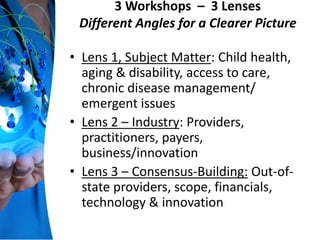
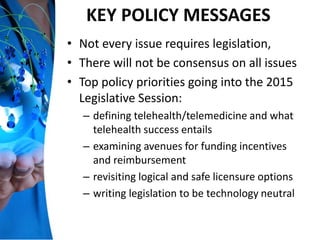
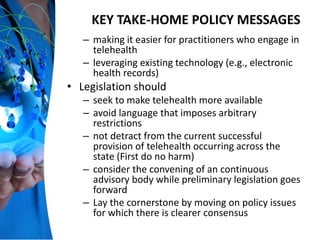
This document summarizes a presentation given at the Florida TeleHealth Summit in Winter Park, Florida on December 5, 2014. The presentation discusses the promise and progress of telehealth, including examples of successful telehealth programs that have reduced costs and hospital readmissions. It also analyzes Florida's efforts and needs regarding telehealth policy, noting the state lags behind others in coverage and reimbursement. The document outlines 42 policy decision points regarding telehealth and emphasizes the importance of telehealth in building a sustainable healthcare system and laying the cornerstone for critical connections to care.