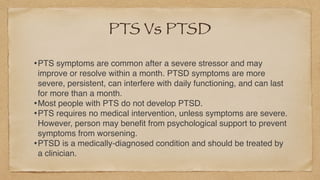
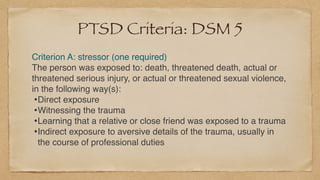
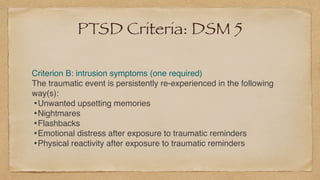
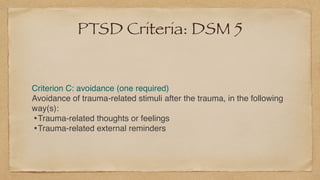
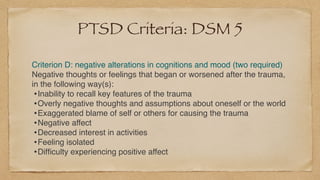
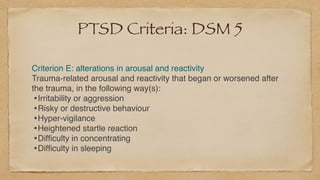
This document discusses dealing with post-traumatic experiences during the COVID-19 pandemic. It defines trauma and outlines common trauma responses like shock, denial, unpredictable emotions, and physical symptoms. It describes acute, chronic, and complex trauma and the five stages of dealing with trauma. Signs of post-traumatic stress (PTS) and post-traumatic stress disorder (PTSD) are provided, along with the DSM-5 criteria for diagnosing PTSD. Effective therapies for PTSD, like cognitive behavioral therapy and its variants, are summarized. The document concludes with suggestions for coping with COVID-19 related trauma, like normalizing experiences, self-care, social connection, and nurturing healthy coping techniques.