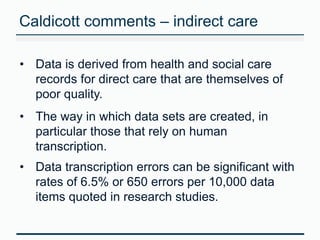
The document emphasizes the critical importance of data quality in health and social care, outlining its role in informed decision-making. It references the Francis and Caldicott reports, which highlight issues with data accuracy and recommend measures such as vigilant local auditing and continuous professional development for providers. The HSCIC's role involves assessing data quality, improving systems, and collaborating with stakeholders to establish a national data quality assurance framework.