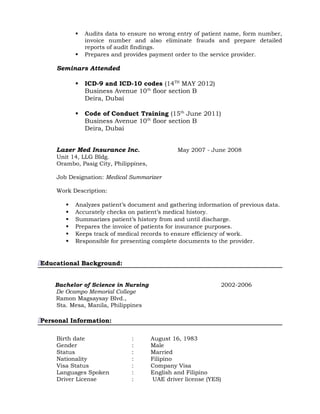
This document contains a summary of Ralph Michael D. Baligod's resume. It lists his objective, qualifications, professional background and education. For his professional background, it details his experience working as a Medical Authorization Executive, Medical Pre-Authorization Executive, Medical Claims Officer, Reimbursement Claims Processor, and Medical Claims Processor/Auditor between 2014-2008 for various companies in Dubai and the Philippines. It also lists his Bachelor of Science in Nursing degree from 2006.