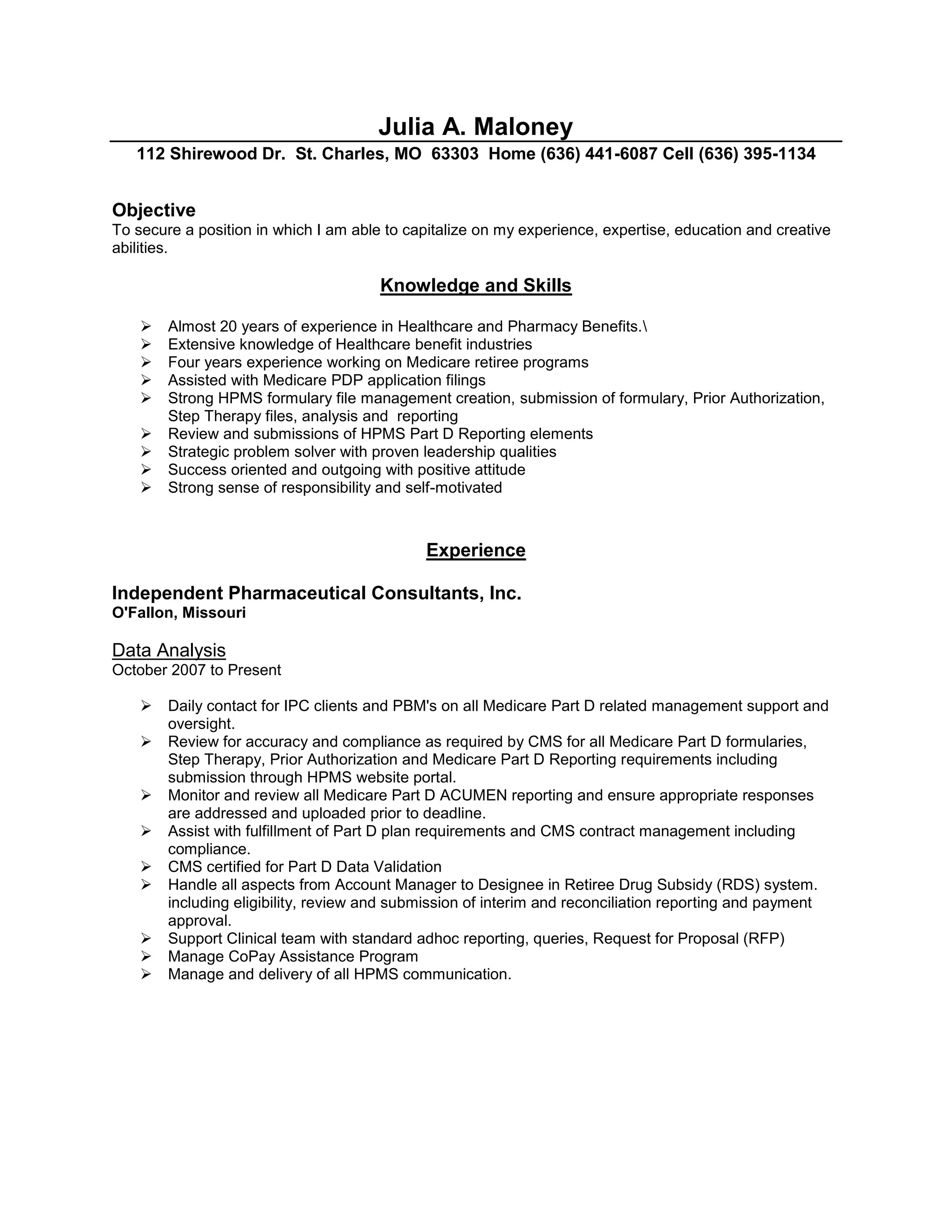
Julia Maloney is seeking a position that utilizes her almost 20 years of experience in healthcare and pharmacy benefits. She has extensive knowledge of healthcare industries and Medicare programs from roles managing Medicare Part D data and ensuring compliance. Maloney has a proven track record of strategic problem solving and leadership with clients and PBMs.