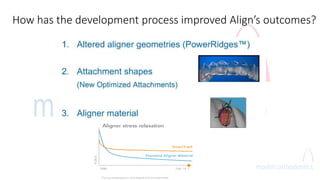
The document discusses the evolution of Invisalign and its advantages over traditional braces, including diagnostic setup for each patient and reducing human error. It also highlights the importance of malocclusion diagnosis, treatment planning, and the factors influencing clinical predictability for successful patient outcomes. Additionally, it addresses tooth size discrepancies and their impact on orthodontic treatment stability and aesthetics.