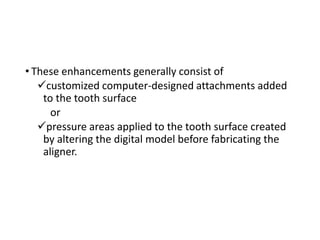
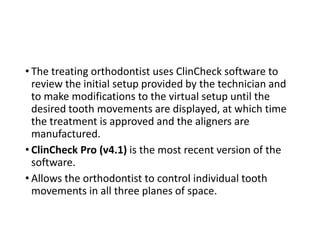
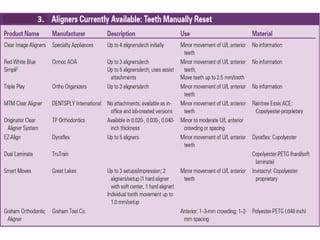
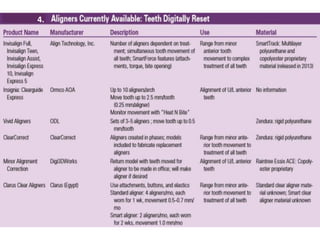
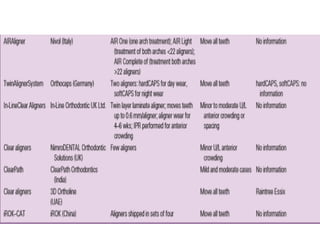
The document provides a comprehensive overview of clear aligner treatment, focusing on invisalign, including its history, techniques, indications, advantages, and limitations. It details advancements in impression techniques and digitization, emphasizing the evolution from manual methods to digital processes, and discusses the classification of aligners and their specific applications. Additionally, it addresses treatment protocols, challenges in patient compliance, and the technological innovations influencing orthodontic practices today.

![INDICATIONS OF INVISALIGN
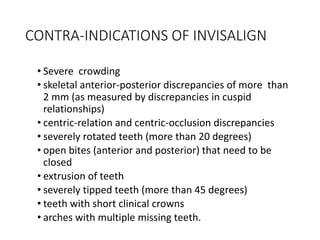
• Joffe L. [Invisalign: early experiences. J Orthod 2003; 30(4):348–52]
suggested that the Invisalign appliance is most successful
for treating:
• mildly malaligned malocclusions (1 to 5 mm of
crowding or spacing)
• deep overbite problems (e.g., Class II division 2
malocclusions) when the overbite can be reduced by
intrusion or advancement of incisors
• nonskeletally constricted arches that can be expanded
with limited tipping of the teeth and mild relapse after
fixed-appliance therapy.](https://image.slidesharecdn.com/cearalignertreatment-210517040919/85/Clear-Aligner-Treatment-21-320.jpg)