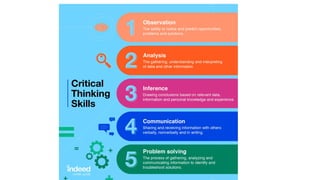
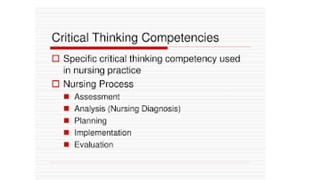
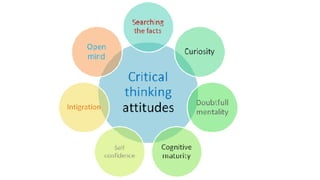
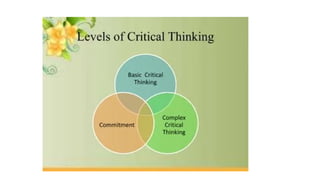
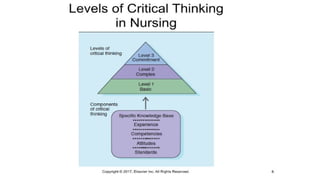
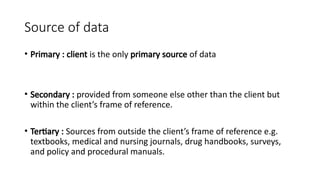
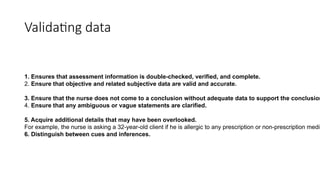
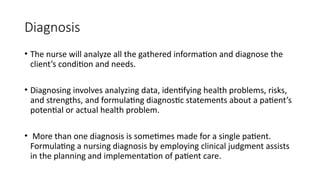
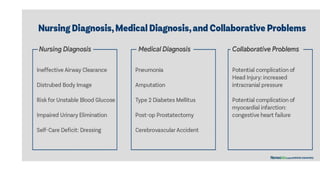
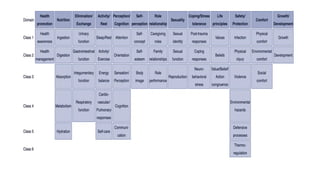
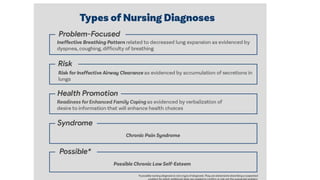
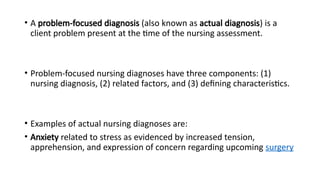
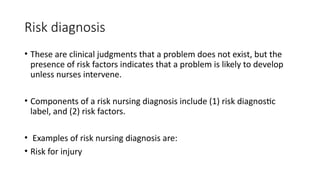
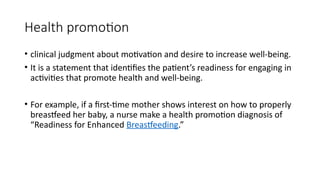
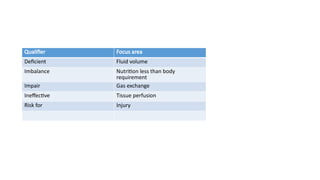
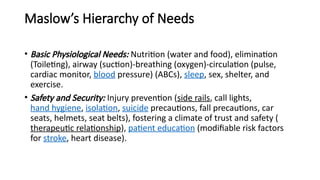
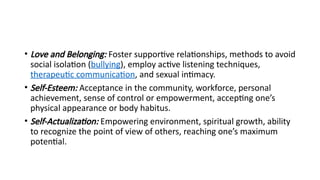
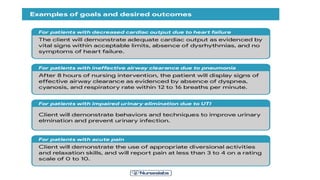
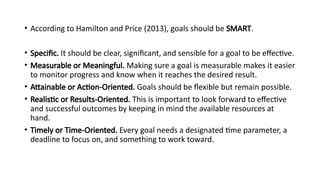
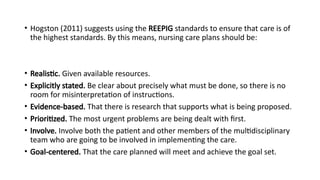
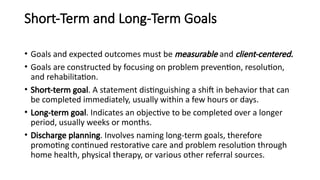
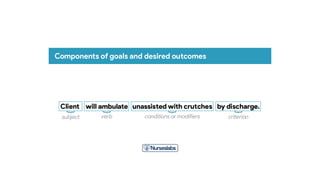
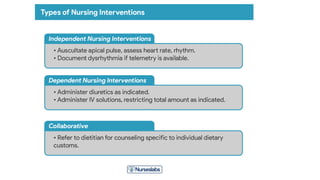
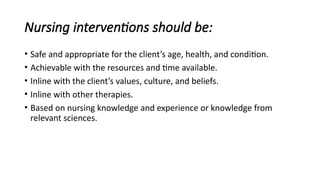
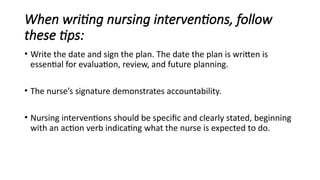
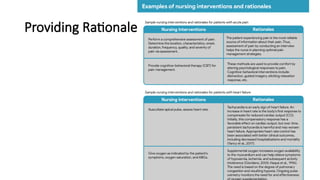
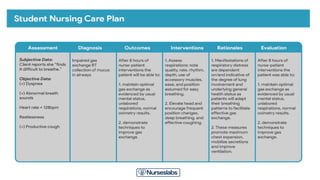
The document outlines the nursing process and critical thinking framework, emphasizing assessment, diagnosis, planning, implementation, and evaluation as key steps in patient care. It discusses the importance of gathering subjective and objective data, formulating nursing diagnoses, setting priorities, and establishing measurable goals for client outcomes. Additionally, it highlights the role of critical thinking in validating data, selecting appropriate interventions, and evaluating the effectiveness of care.