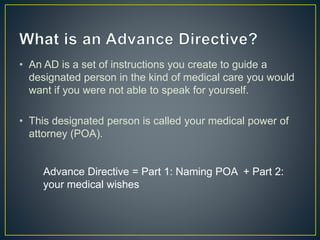
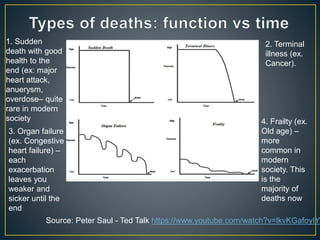
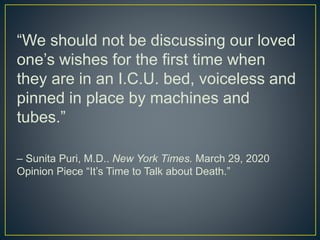
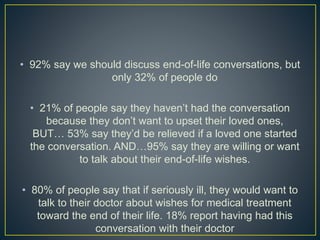
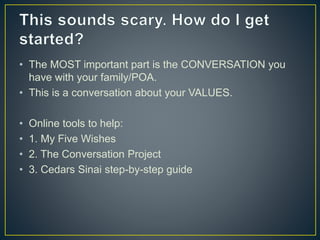
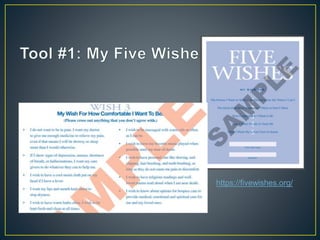
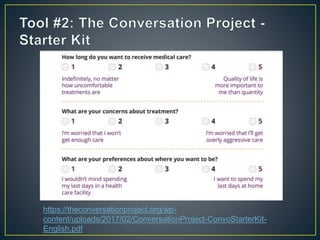
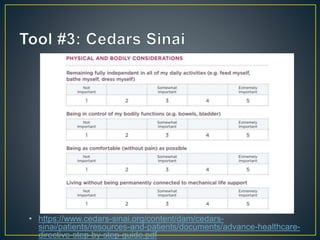
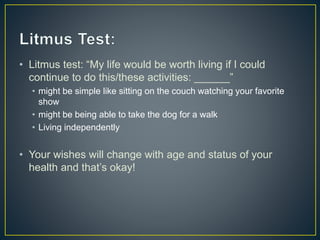
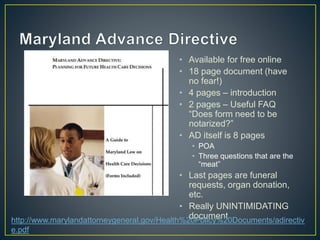
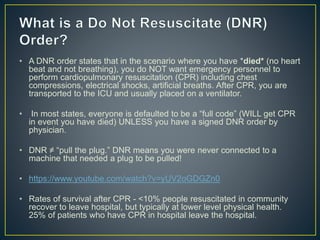
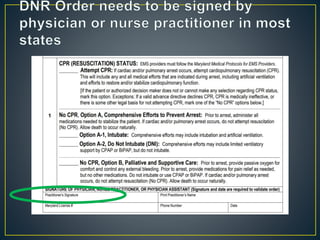
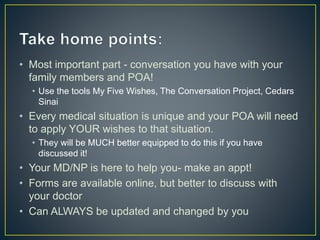
This document discusses advance directives and the importance of planning for end-of-life medical care. It explains that an advance directive allows a person to designate a medical power of attorney and outline their medical wishes if they become unable to communicate. It emphasizes having conversations with family and medical providers about one's values and priorities for care. The document provides resources for creating advance directives and discusses do not resuscitate (DNR) orders and other key end-of-life decisions.