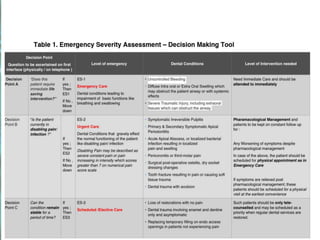
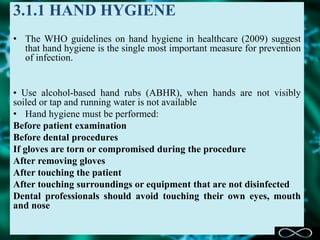
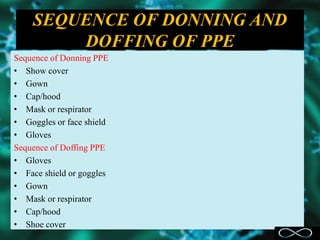
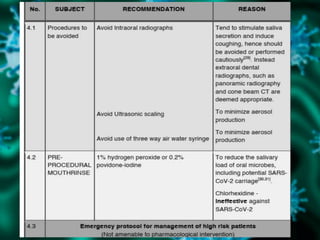
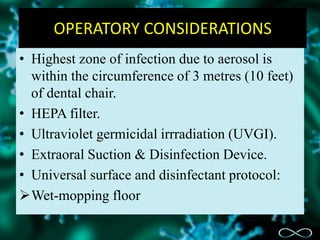
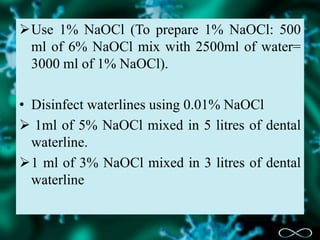
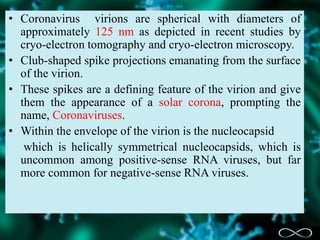
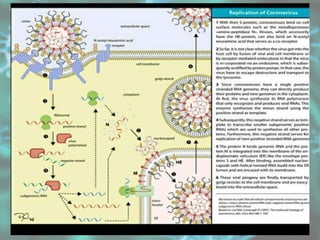
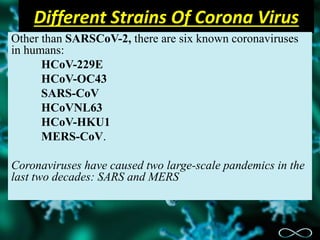
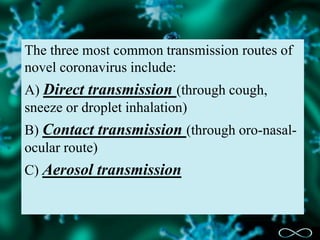
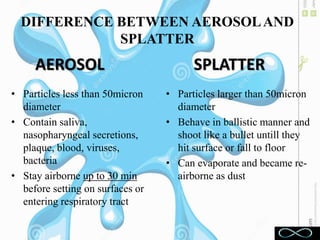
The document discusses COVID-19, focusing on its characteristics, transmission routes, symptoms, diagnosis, and management strategies for patients, particularly in dental settings. It highlights the challenges posed by asymptomatic carriers and the importance of infection control measures, including triaging patients and the use of personal protective equipment. Recommendations for managing dental care during the pandemic are provided to ensure safety for patients and healthcare providers alike.









![According to standards protocol of
WHO
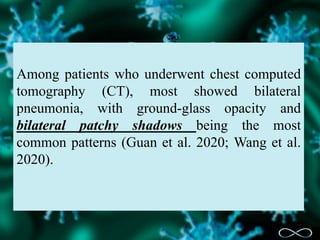
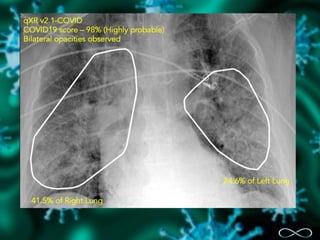
The diagnosis of COVID-19 can be based on a
combination of epidemiologic information (e.g., a history
of travel to or residence in affected region 14 days prior to
symptom onset), clinical symptoms, CT imaging findings,
and laboratory tests (e.g., reverse transcriptase polymerase
chain reaction [RT-PCR] tests on respiratory tract
specimens)](https://image.slidesharecdn.com/covid19-200418193238/85/Covid-19-EMERGING-AND-FUTURE-CHALLENGES-FOR-DENTAL-SURGEON-34-320.jpg)

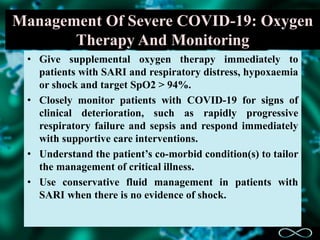
![Management Of Critical Illness And
COVID-19: Septic Shock
• Recognize septic shock in adults when infection is suspected or
confirmed & vasopressors are needed to maintain mean arterial
pressure (MAP) ≥ 65 mmHg & lactate is ≥ 2 mmol/L, in absence
of hypovolemia.
• Recognize septic shock in children with any hypotension
(systolic blood pressure [SBP] < 5th centile or > 2 SD below
normal for age) or two or more of the following: altered mental
state; bradycardia or tachycardia (HR < 90 bpm or > 160 bpm
in infants and HR < 70 bpm or > 150 bpm in children);
prolonged capillary refill (> 2 sec) or feeble pulses; tachypnea;
mottled or cold skin or petechial or purpuric rash; increased
lactate; oliguria; hyperthermia or hypothermia.](https://image.slidesharecdn.com/covid19-200418193238/85/Covid-19-EMERGING-AND-FUTURE-CHALLENGES-FOR-DENTAL-SURGEON-41-320.jpg)