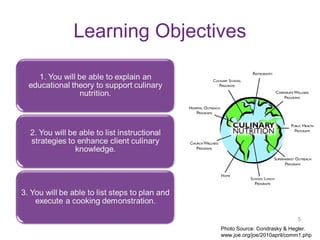
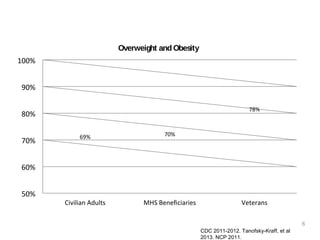
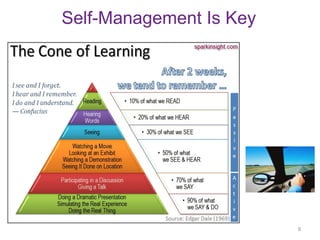
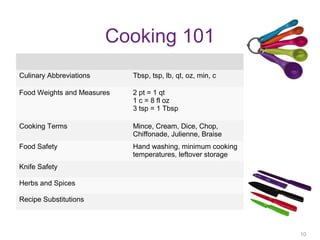
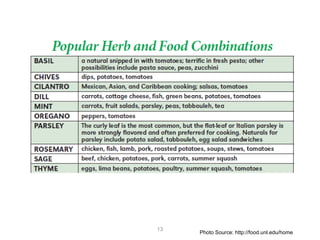
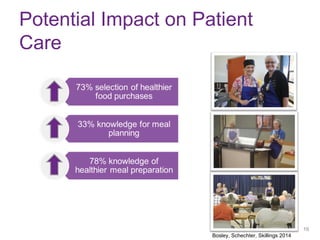
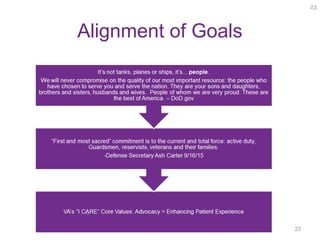
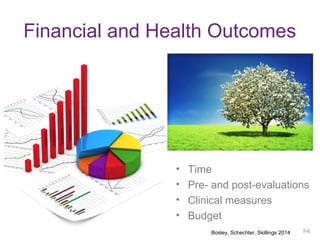
This document outlines a nutrition education program aimed at military families, highlighting the importance of cooking skills and culinary education in promoting healthy eating habits. It emphasizes the use of evidence-based practices and adult learning theories to enhance program effectiveness and improve outcomes. The document also includes resources, strategies, and evaluations to support culinary education efforts in various settings.