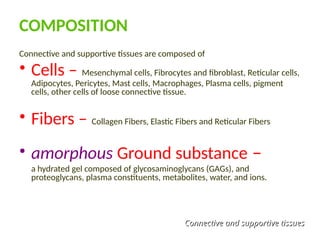
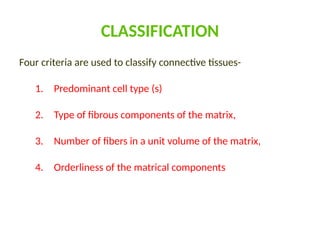
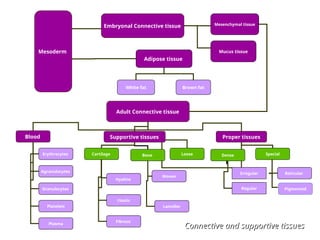
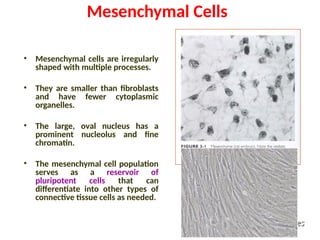
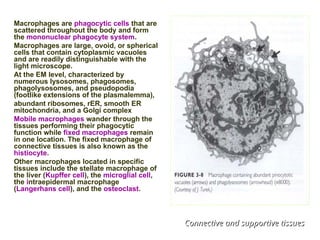
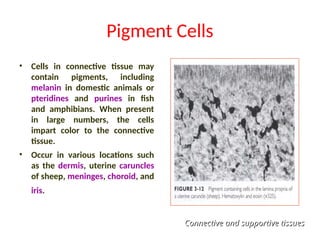
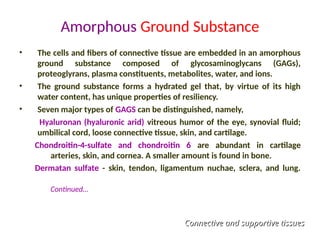
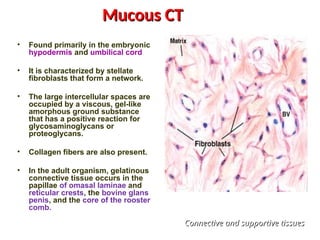
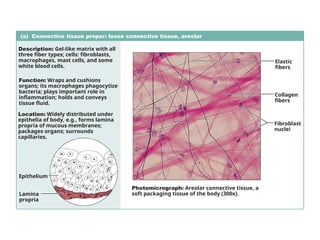
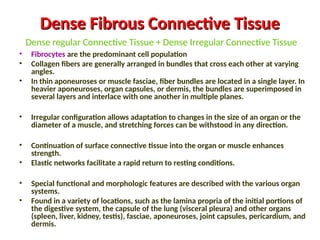
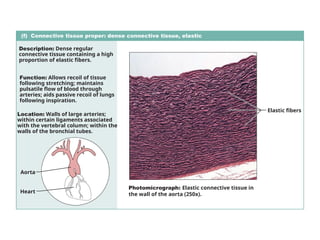
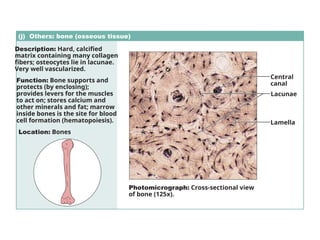
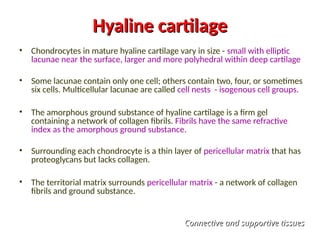
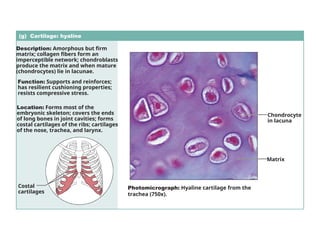
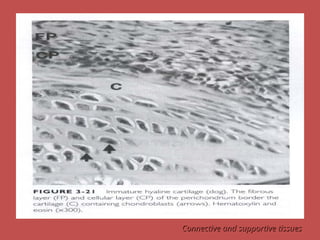
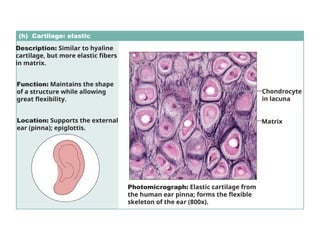
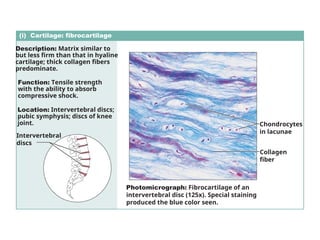
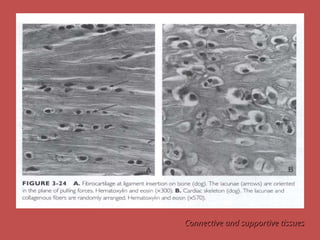
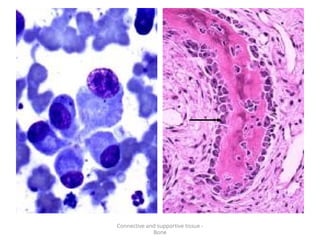
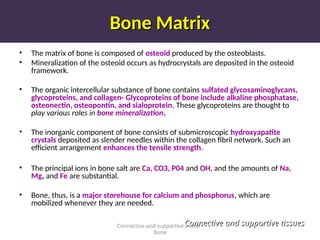
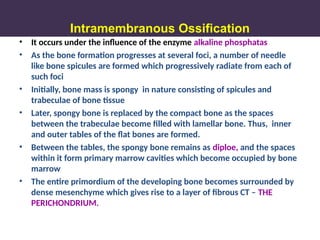
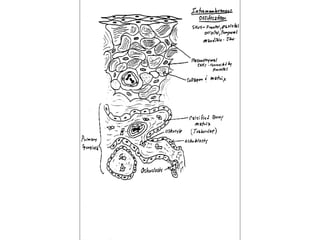
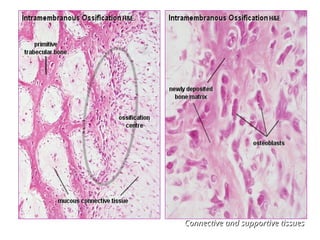
Connective and supportive tissues serve key functions such as connecting other tissues, providing a structural framework, and playing roles in thermoregulation and repair mechanisms. These tissues are composed of various cells (e.g., fibroblasts, adipocytes) and fibers (e.g., collagen, elastic), leading to classifications based on cell types and matrix composition. Key components include fixed and wandering cells, types of fibers, and amorphous ground substance, with specific functionalities in various connective tissue types like loose, dense, and embryonic tissues.