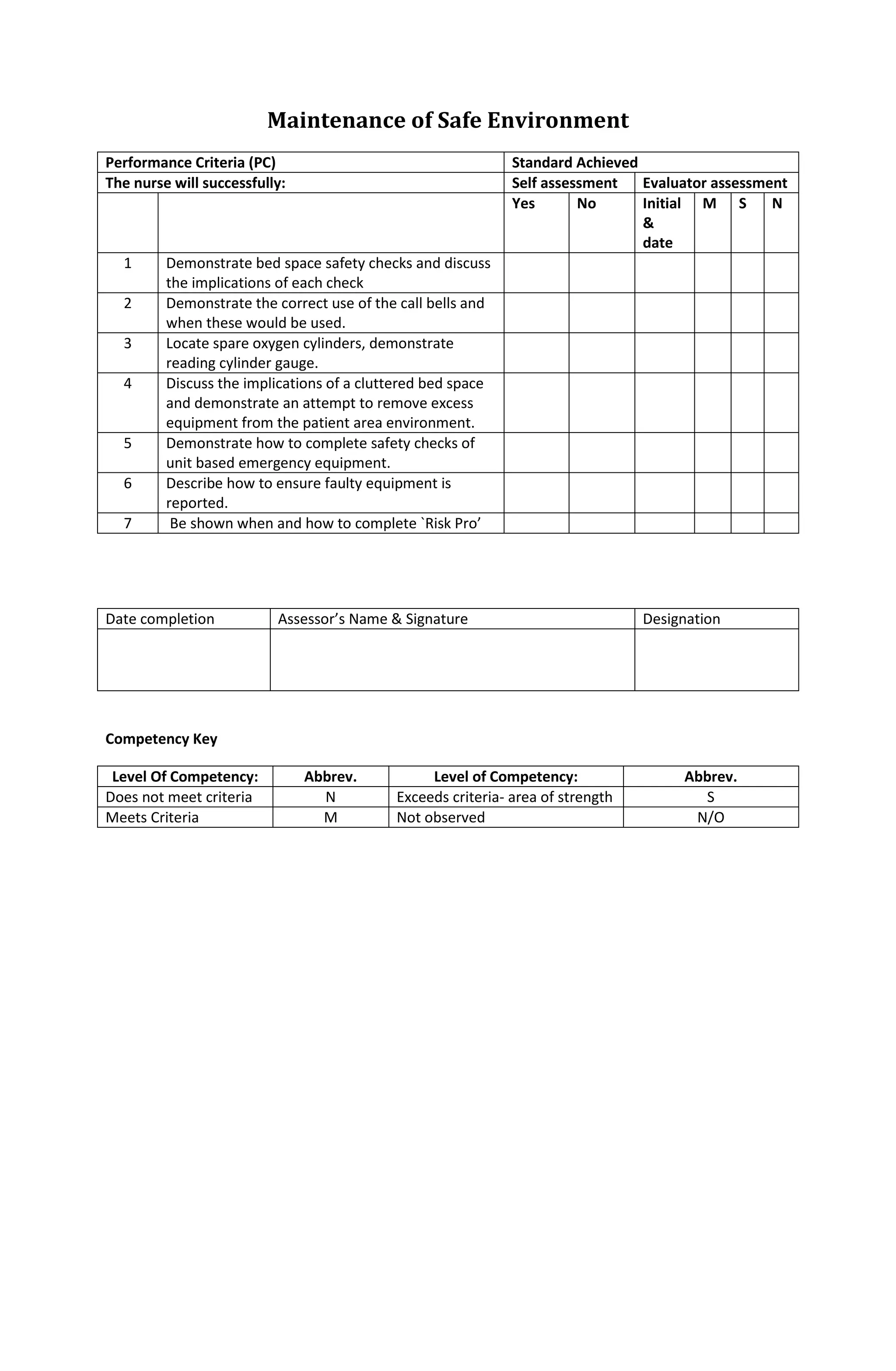
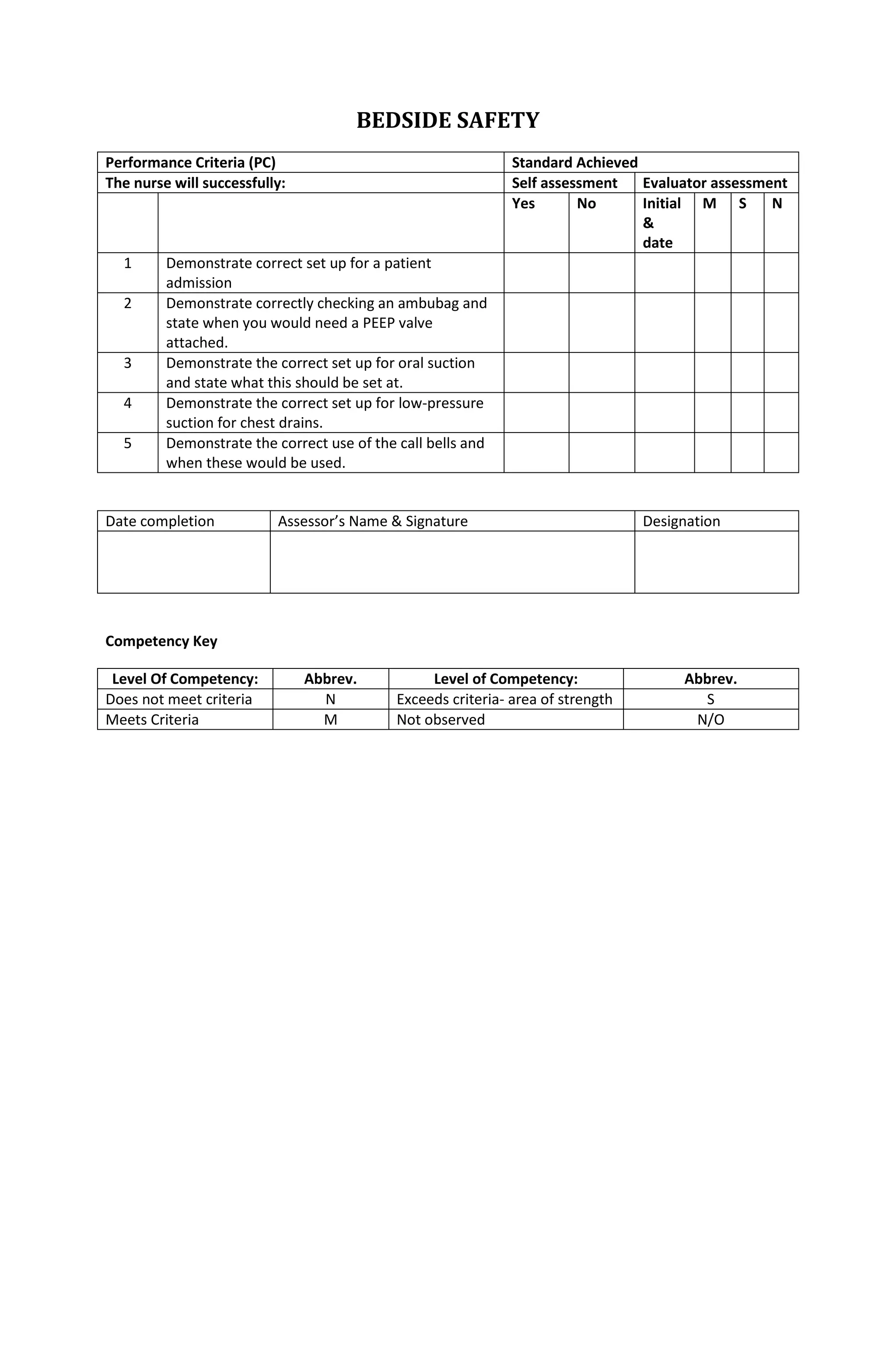
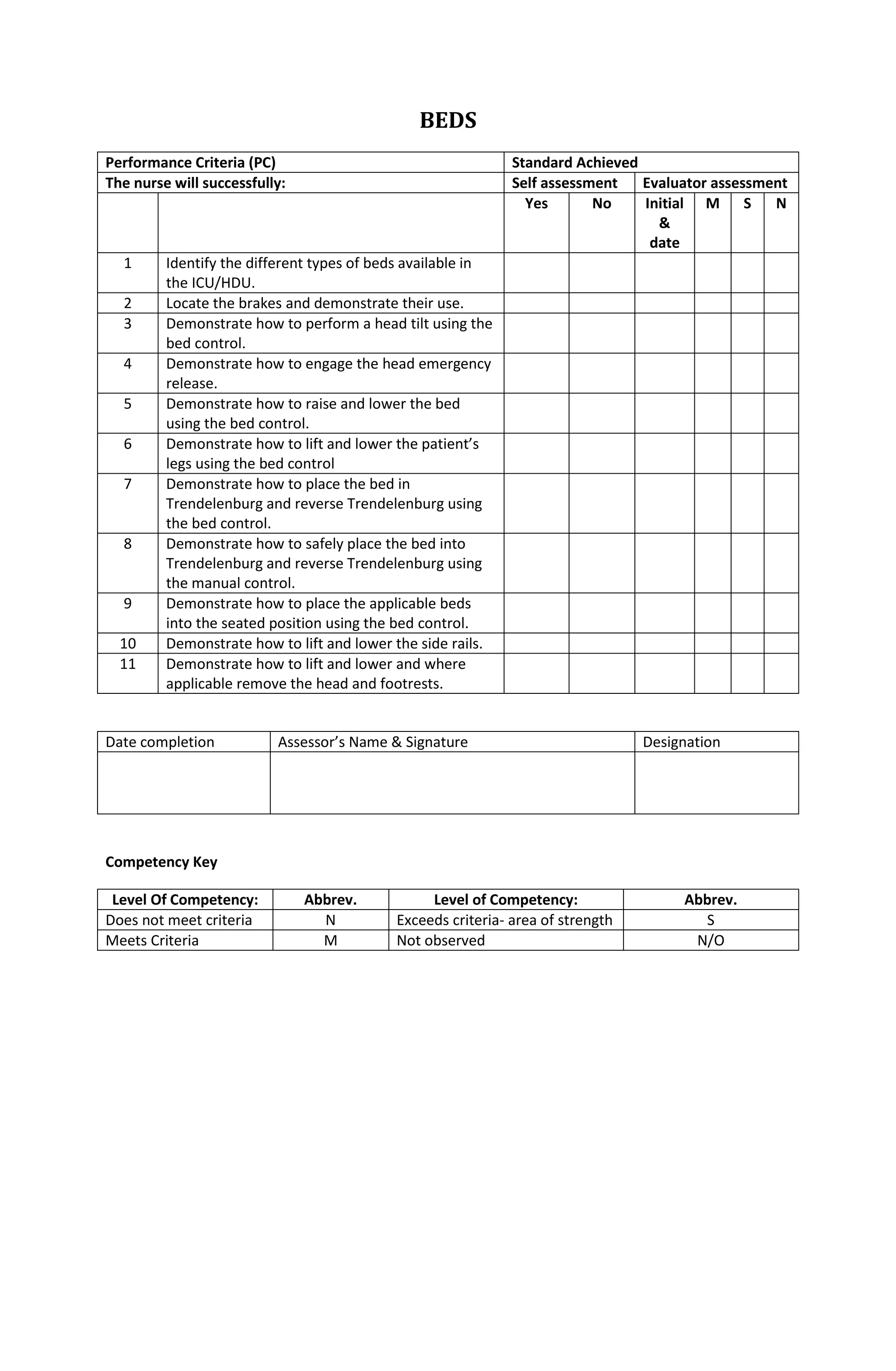
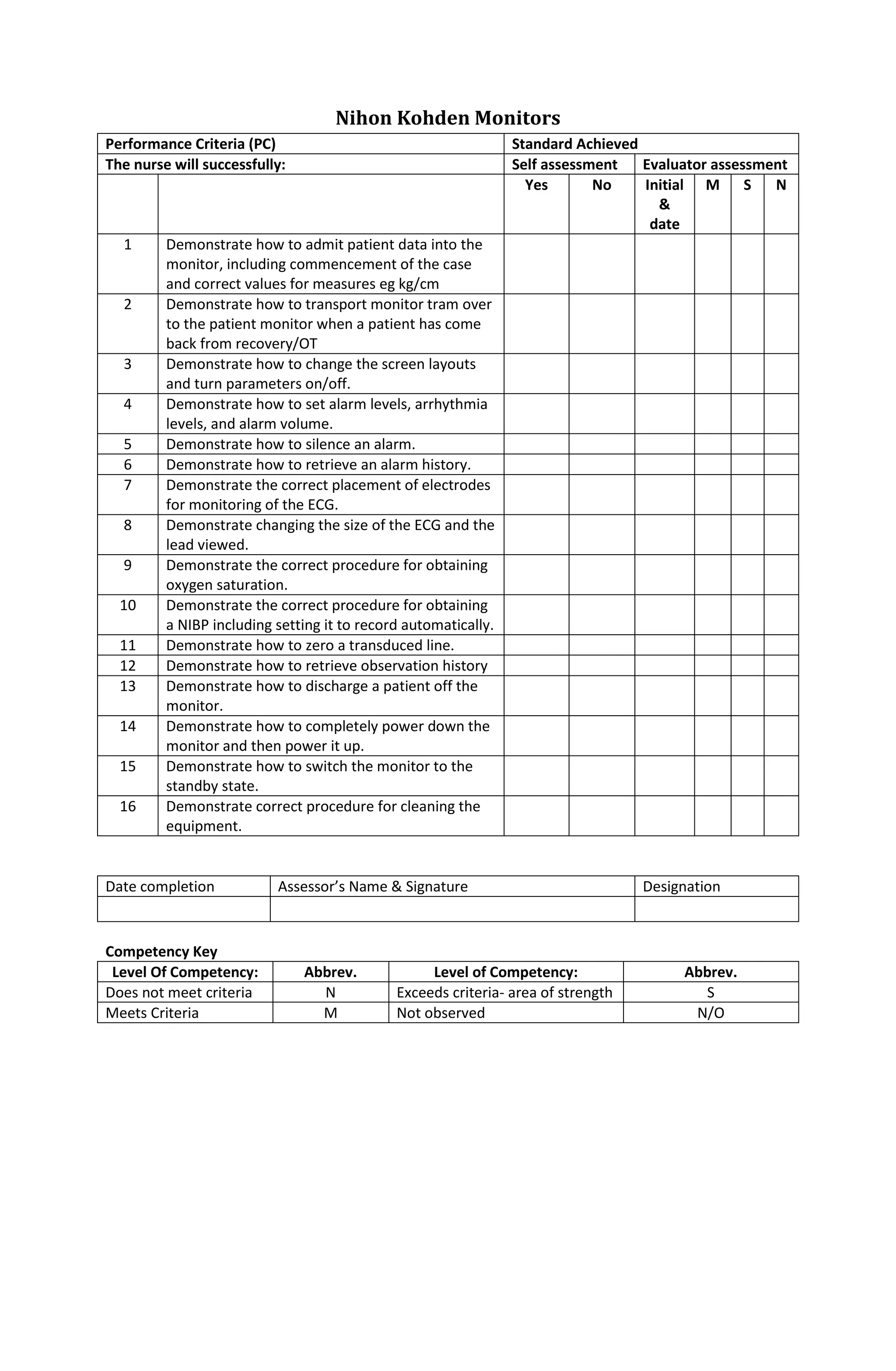
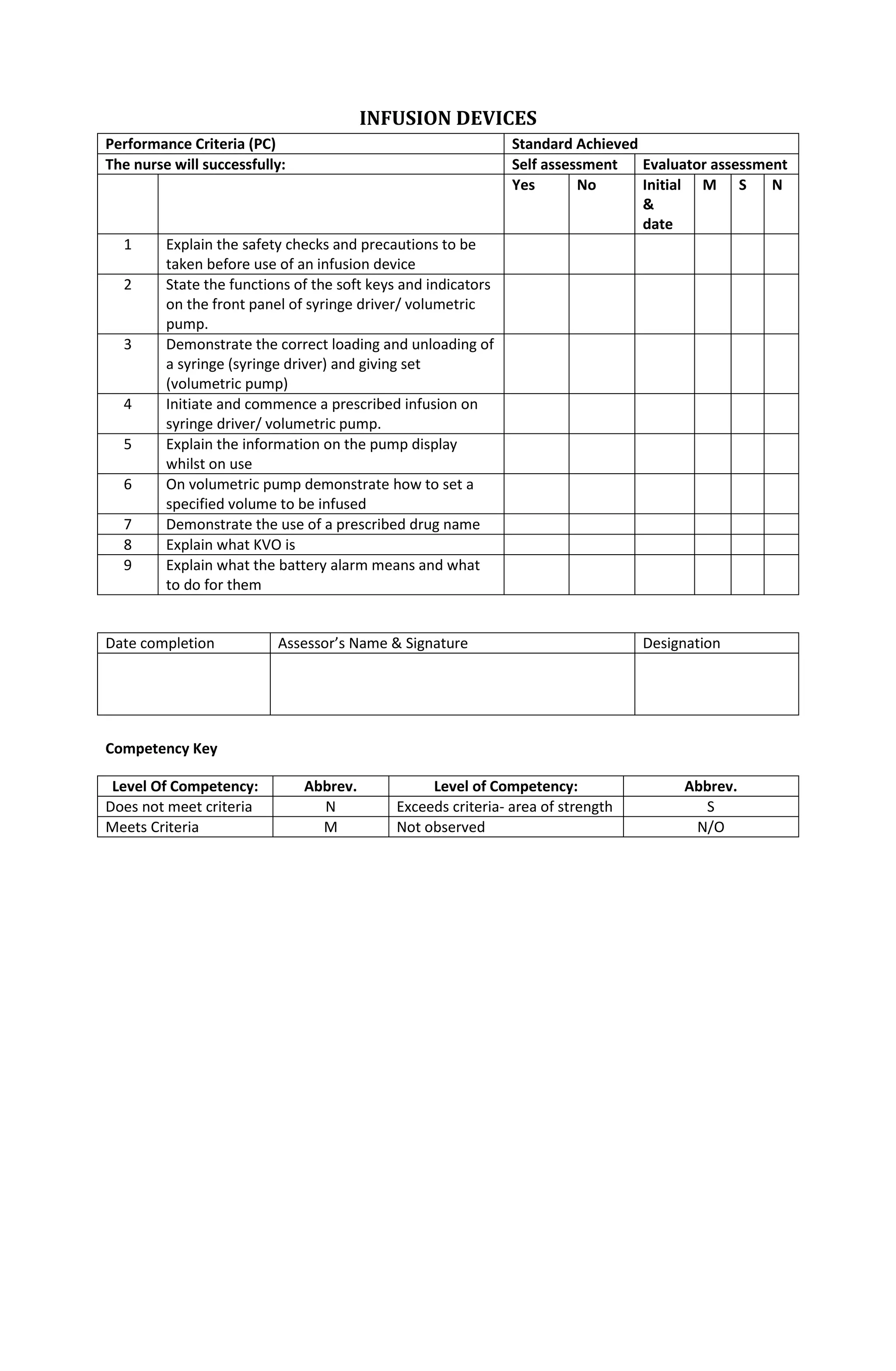
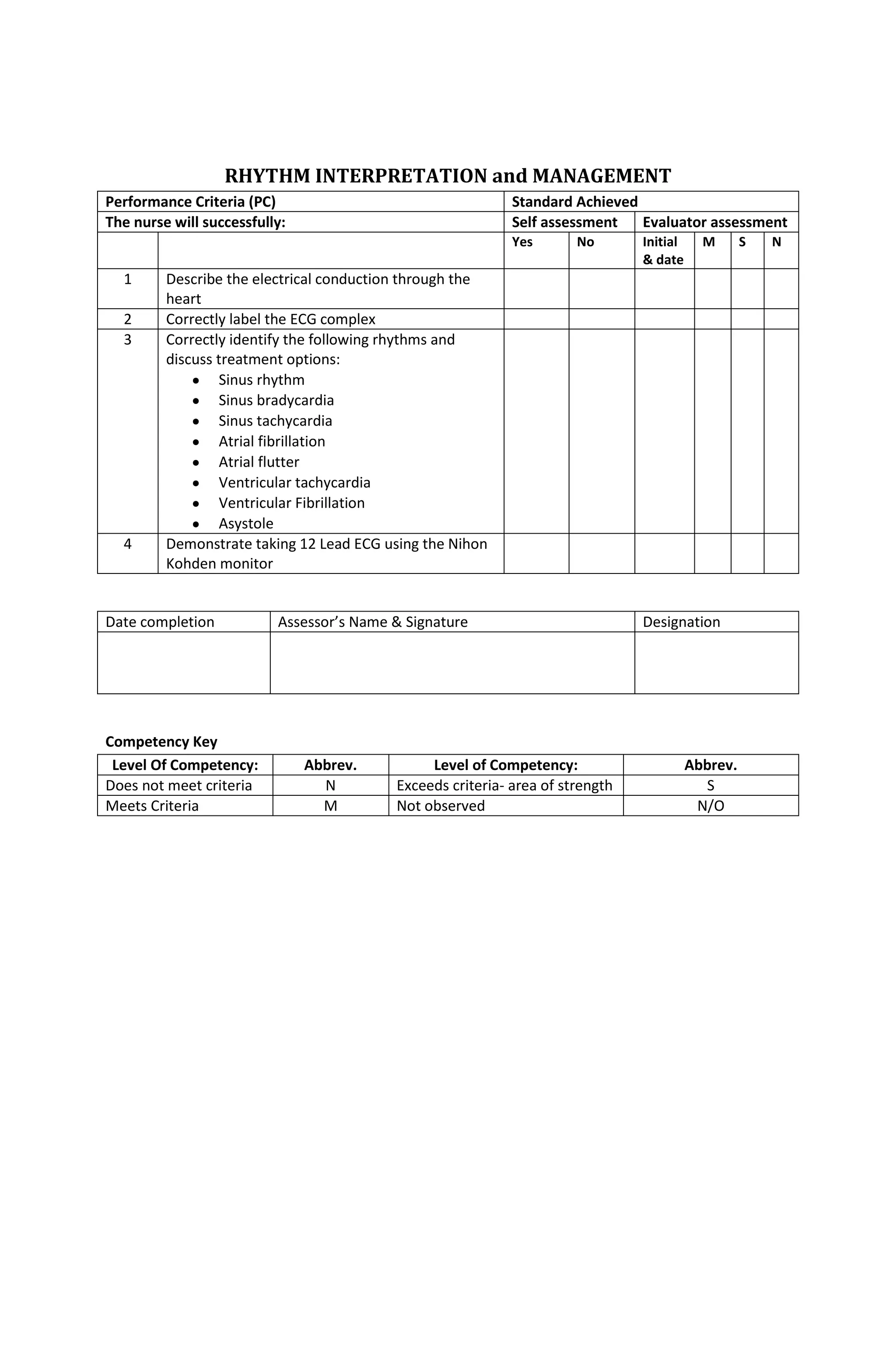
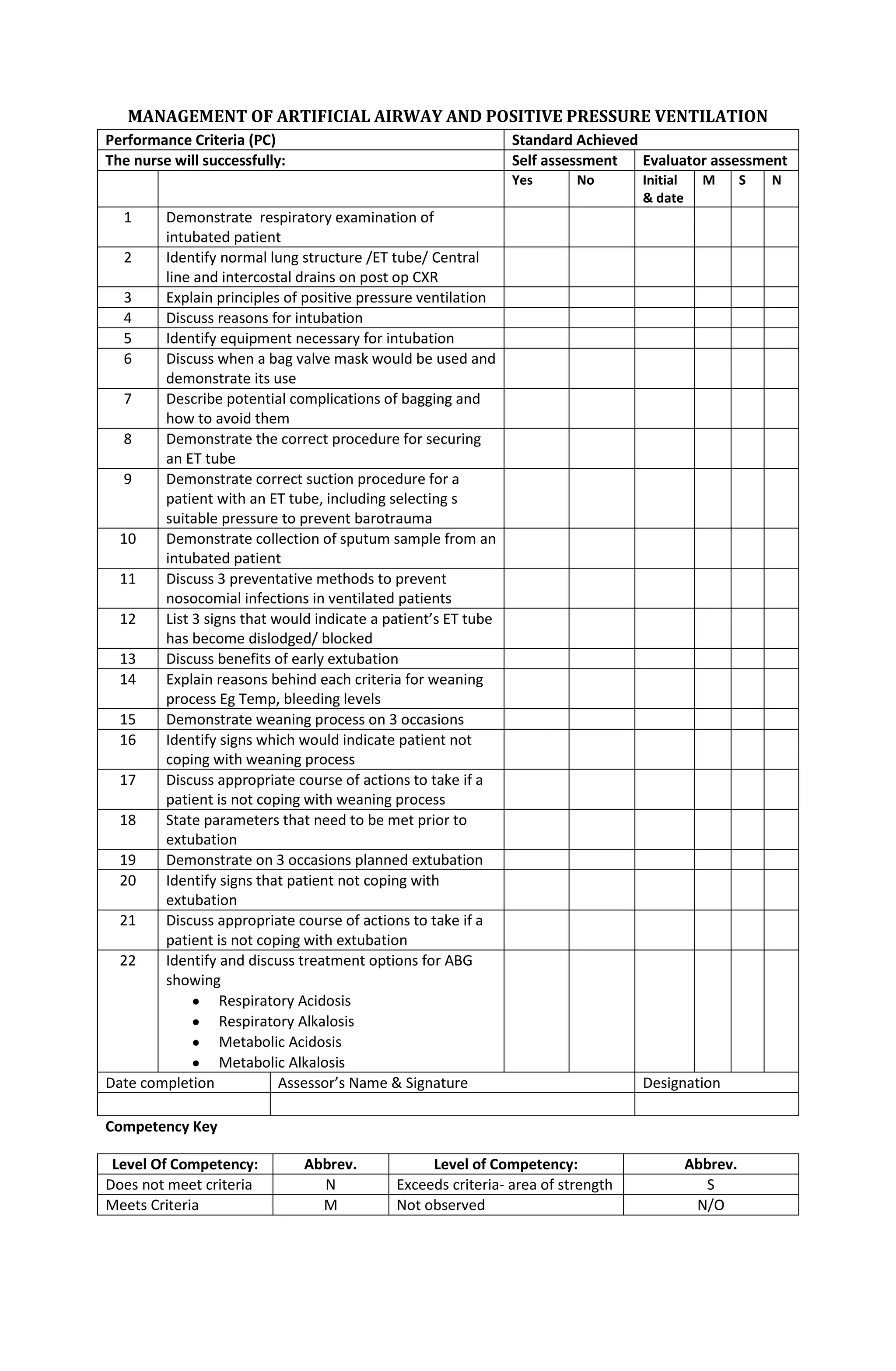
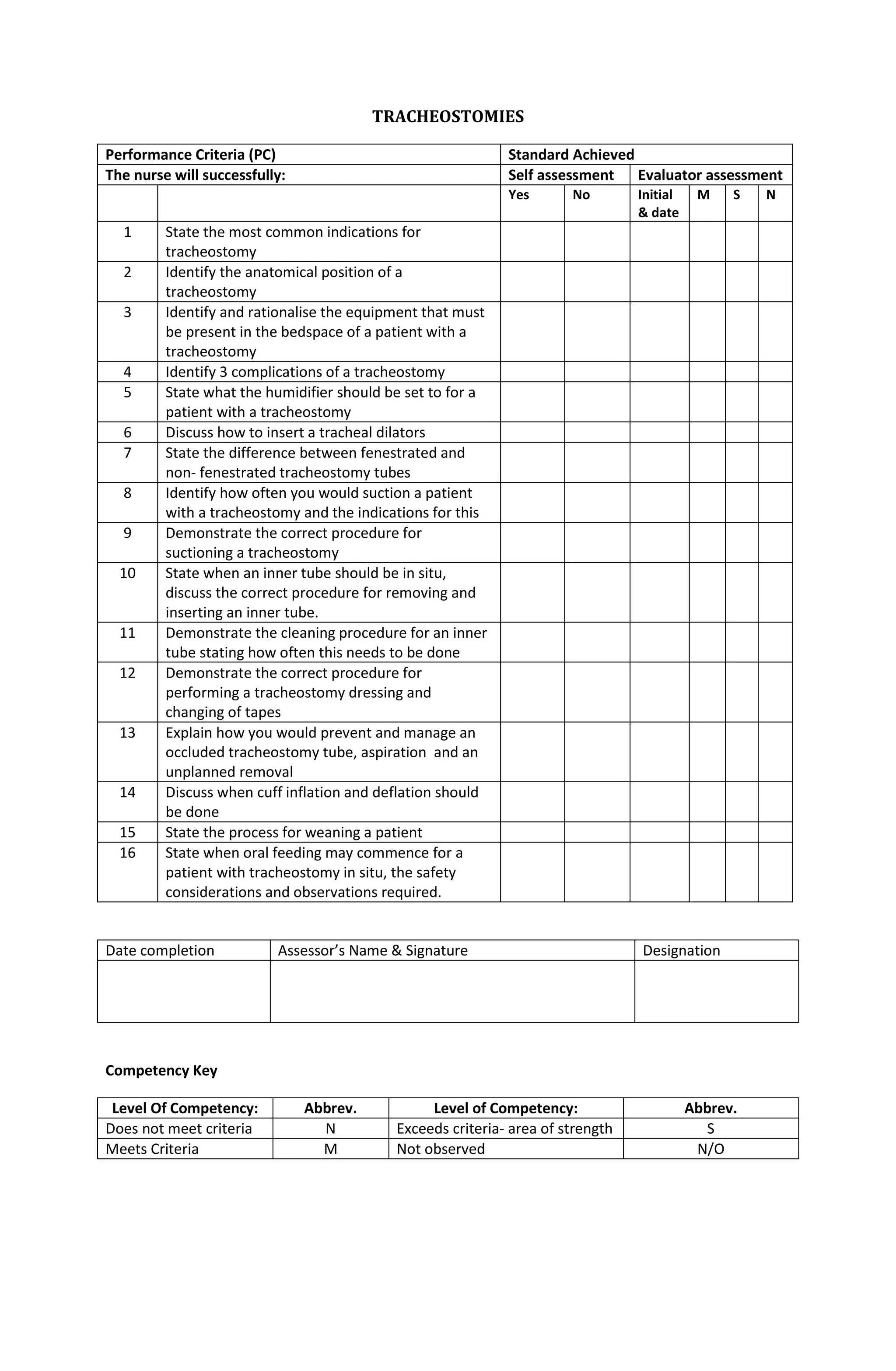
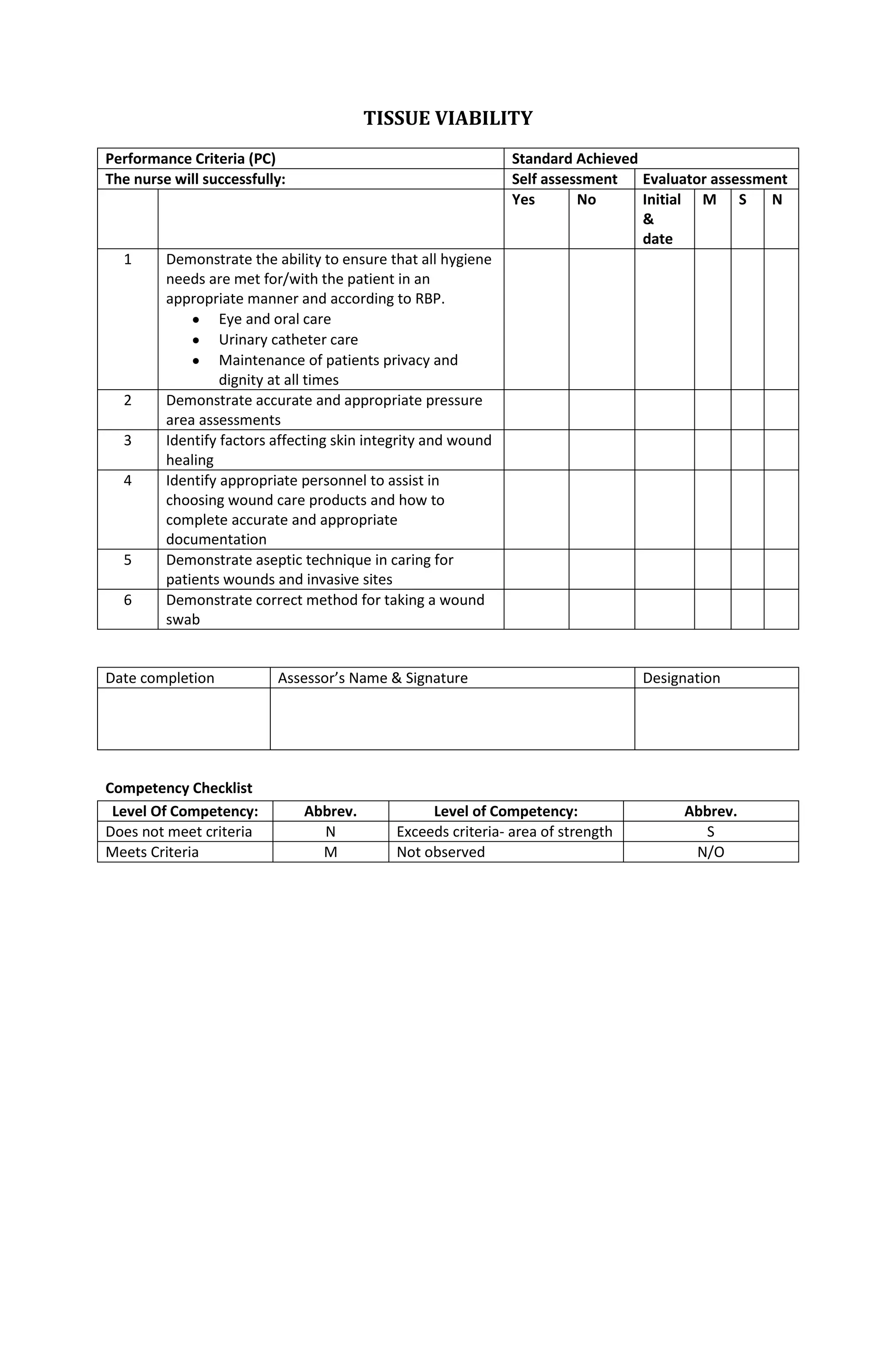
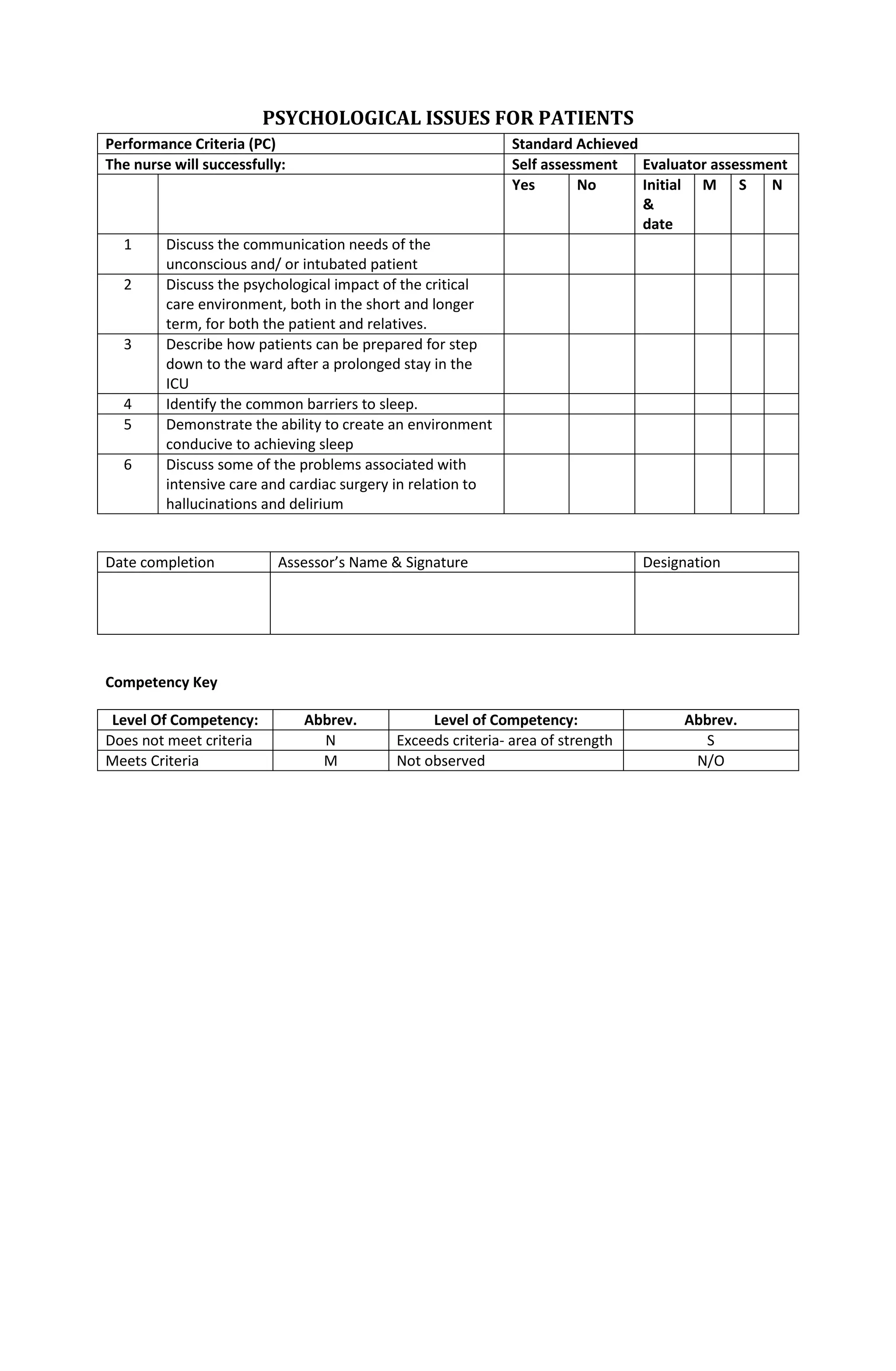
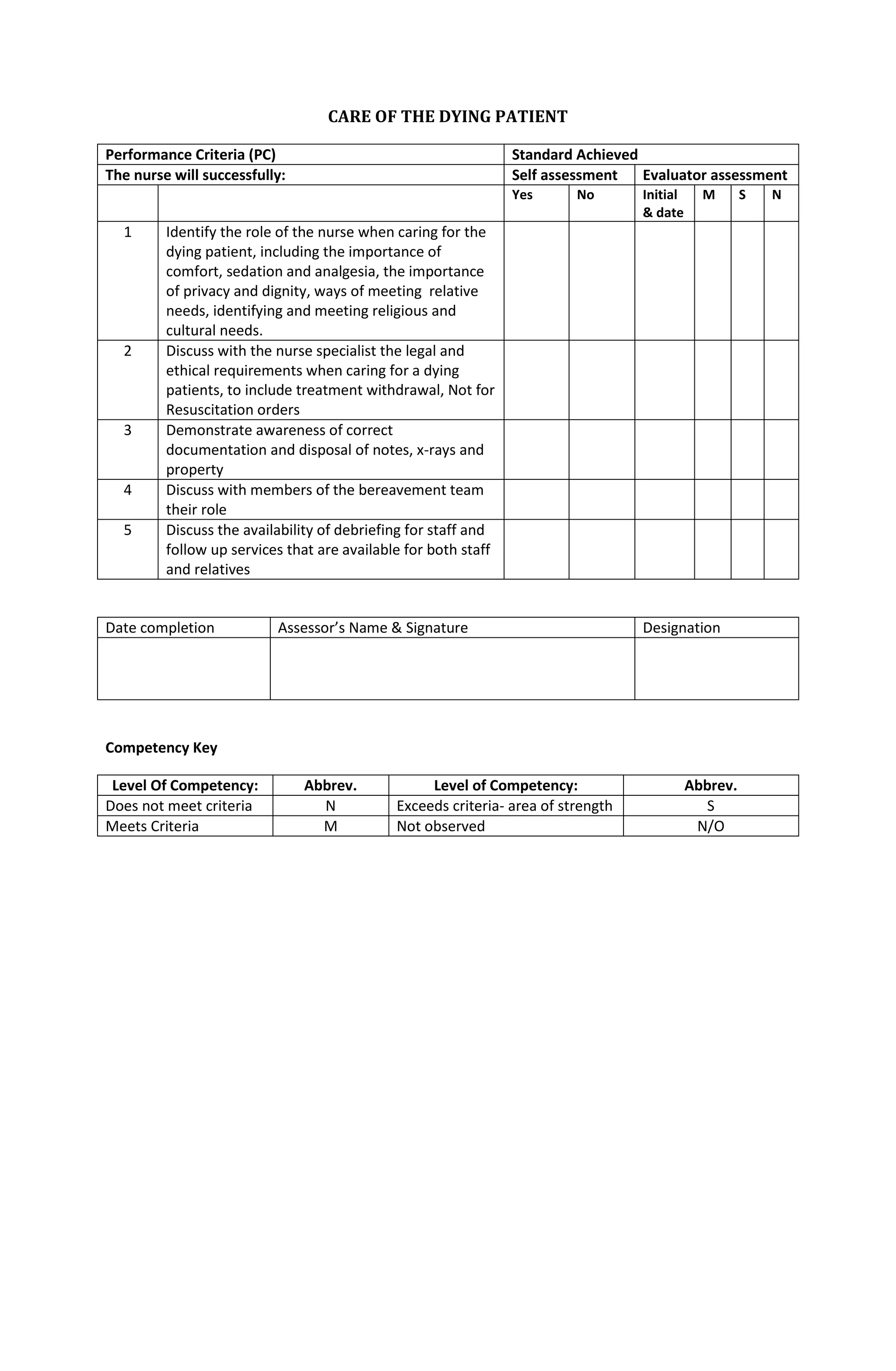
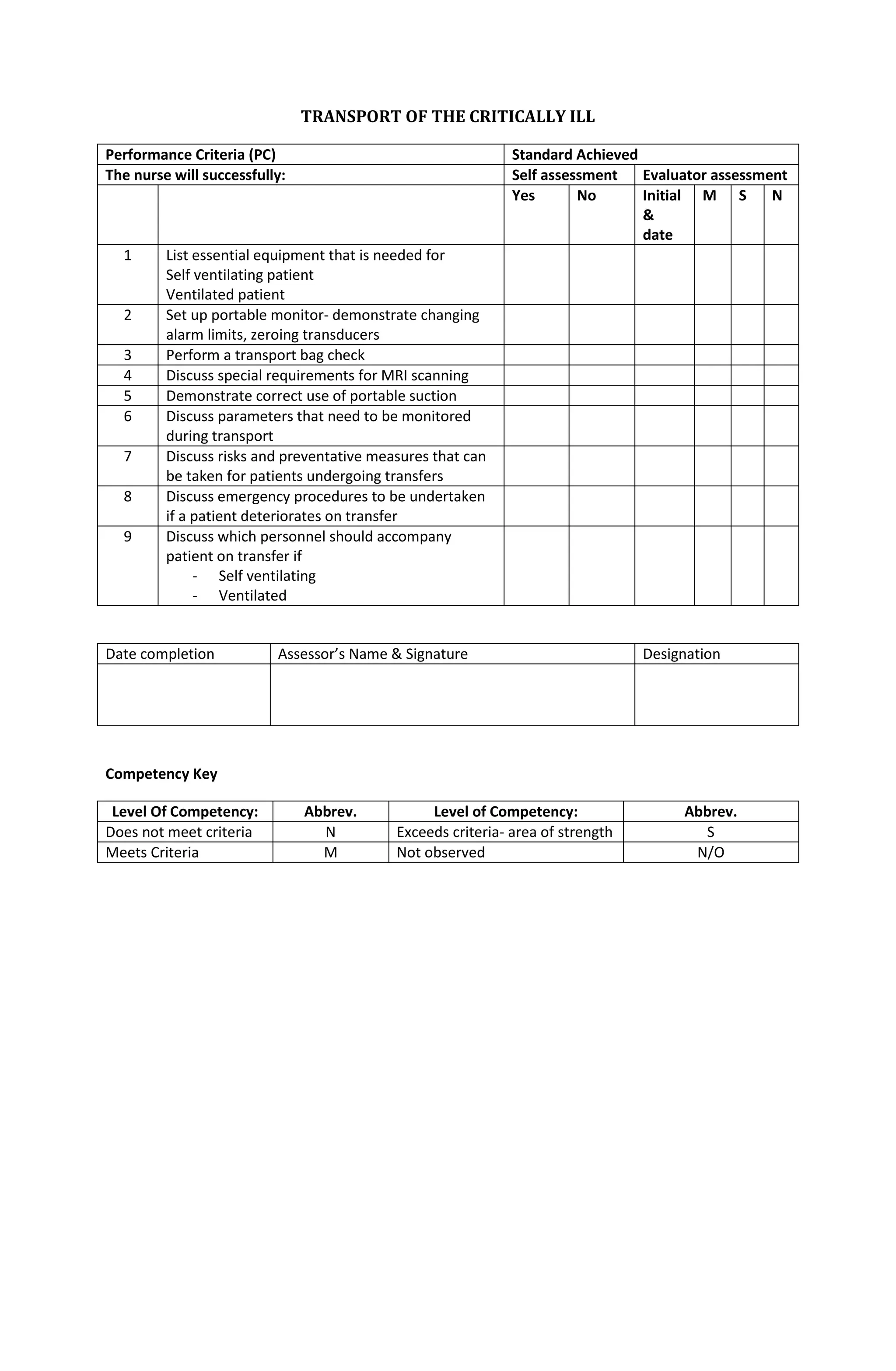
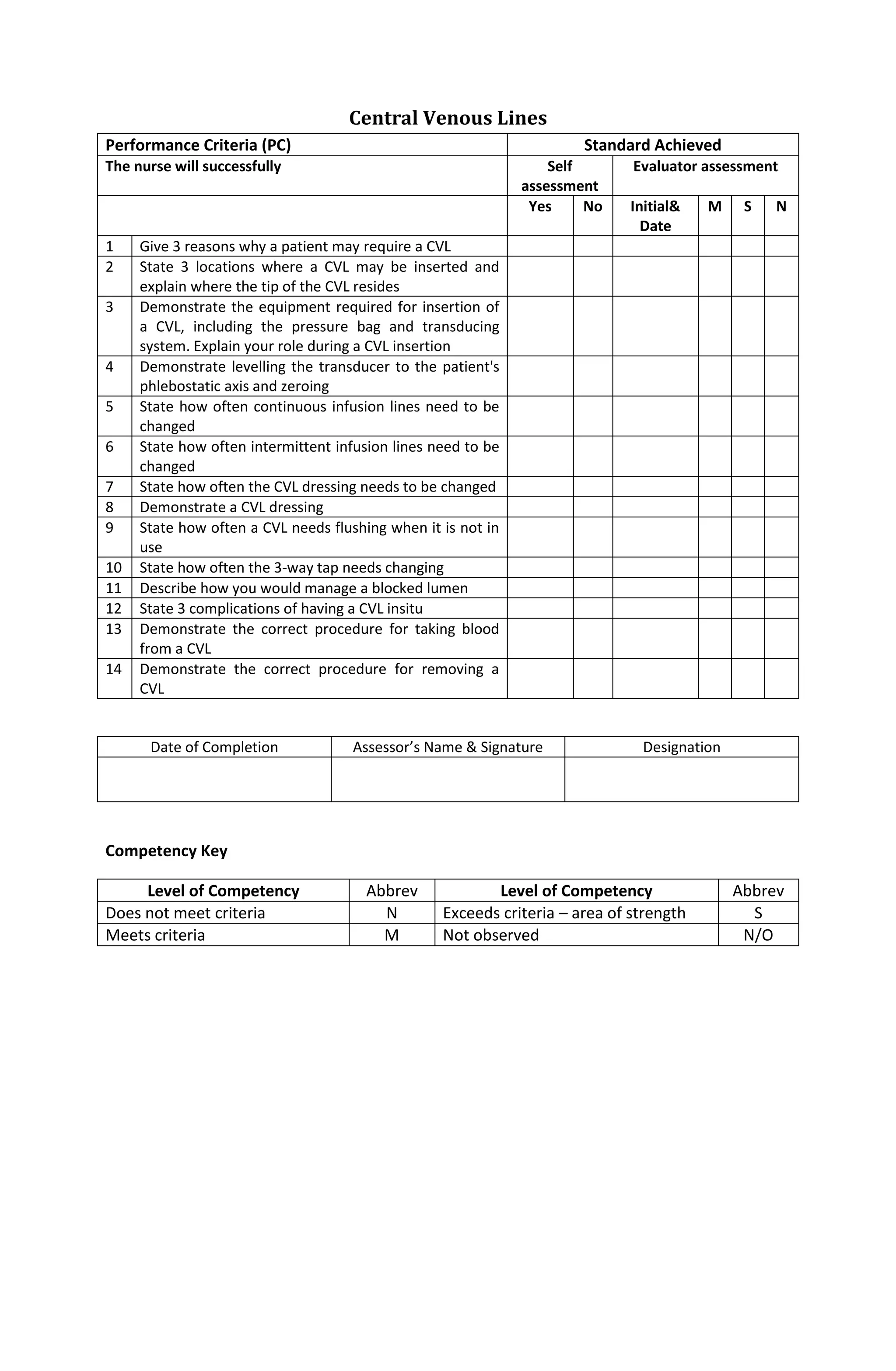
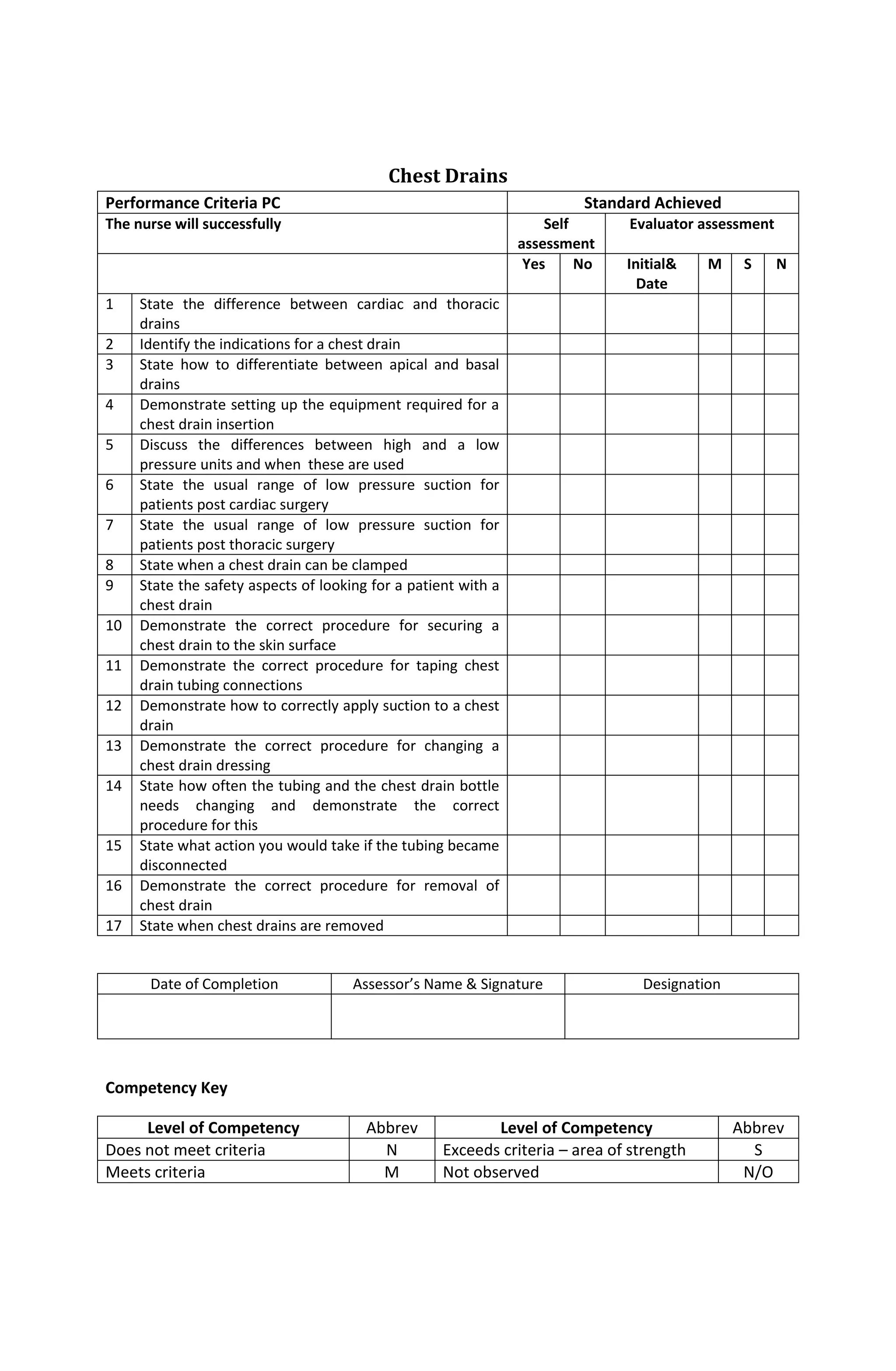
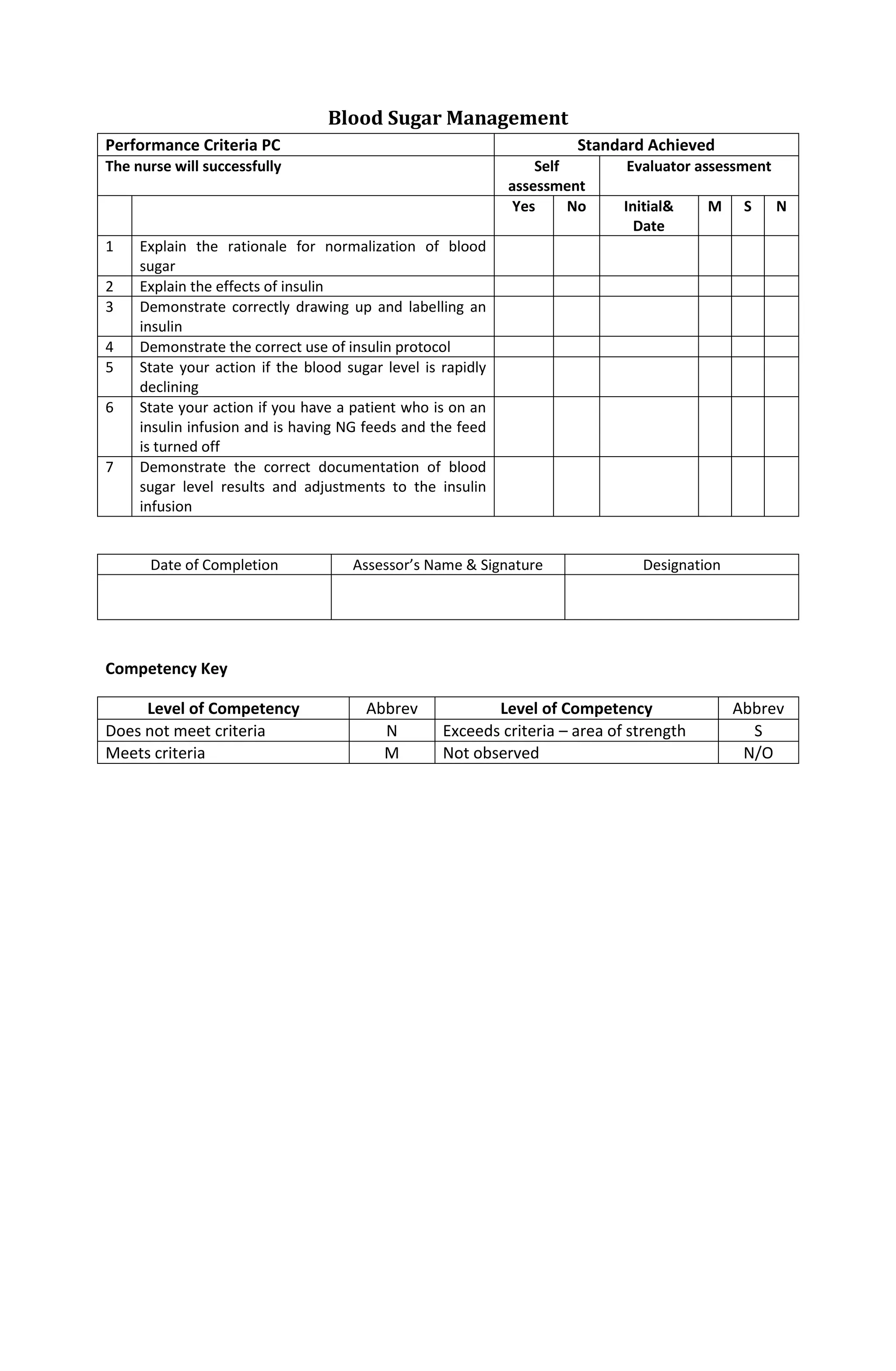
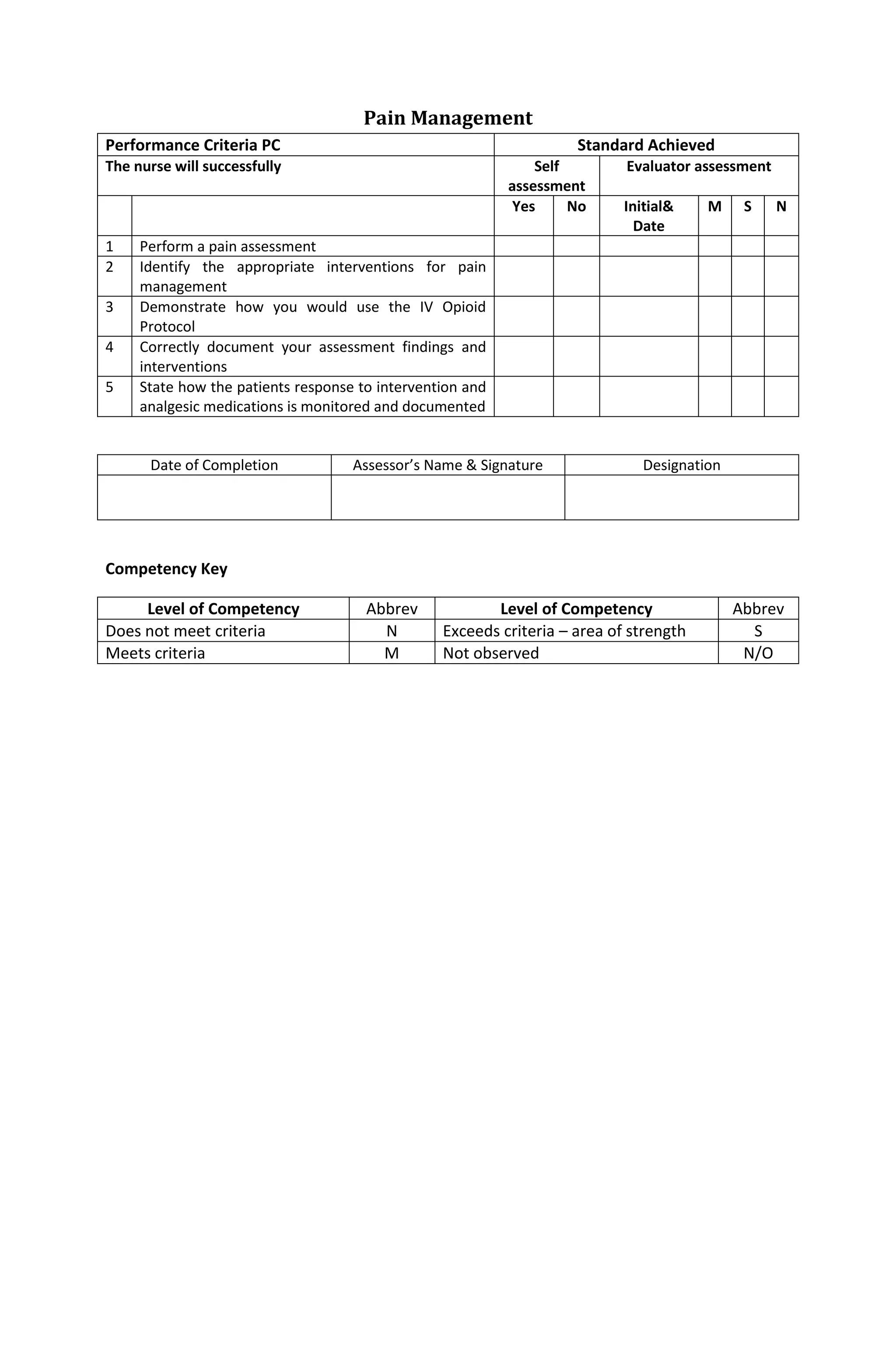
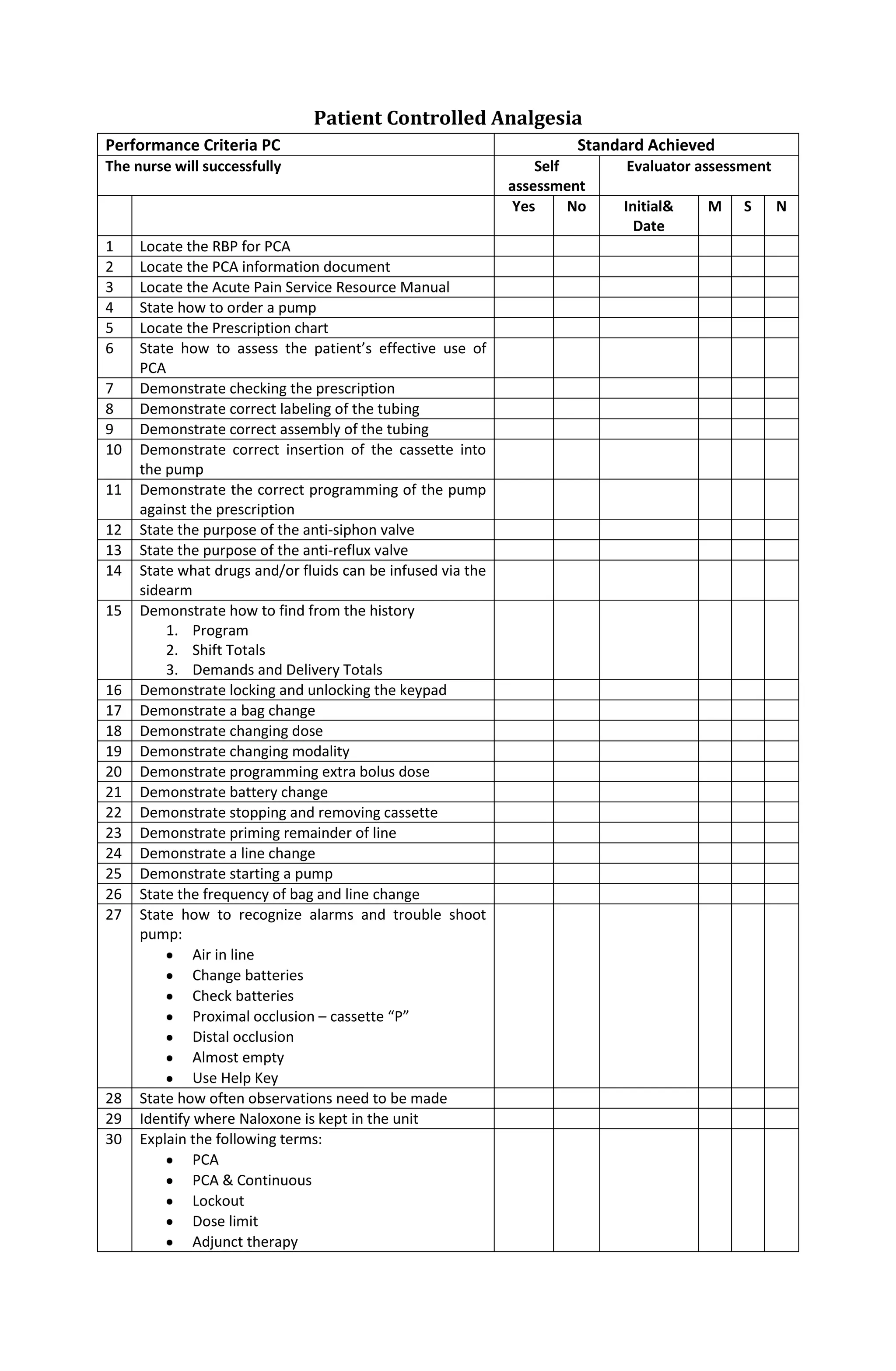
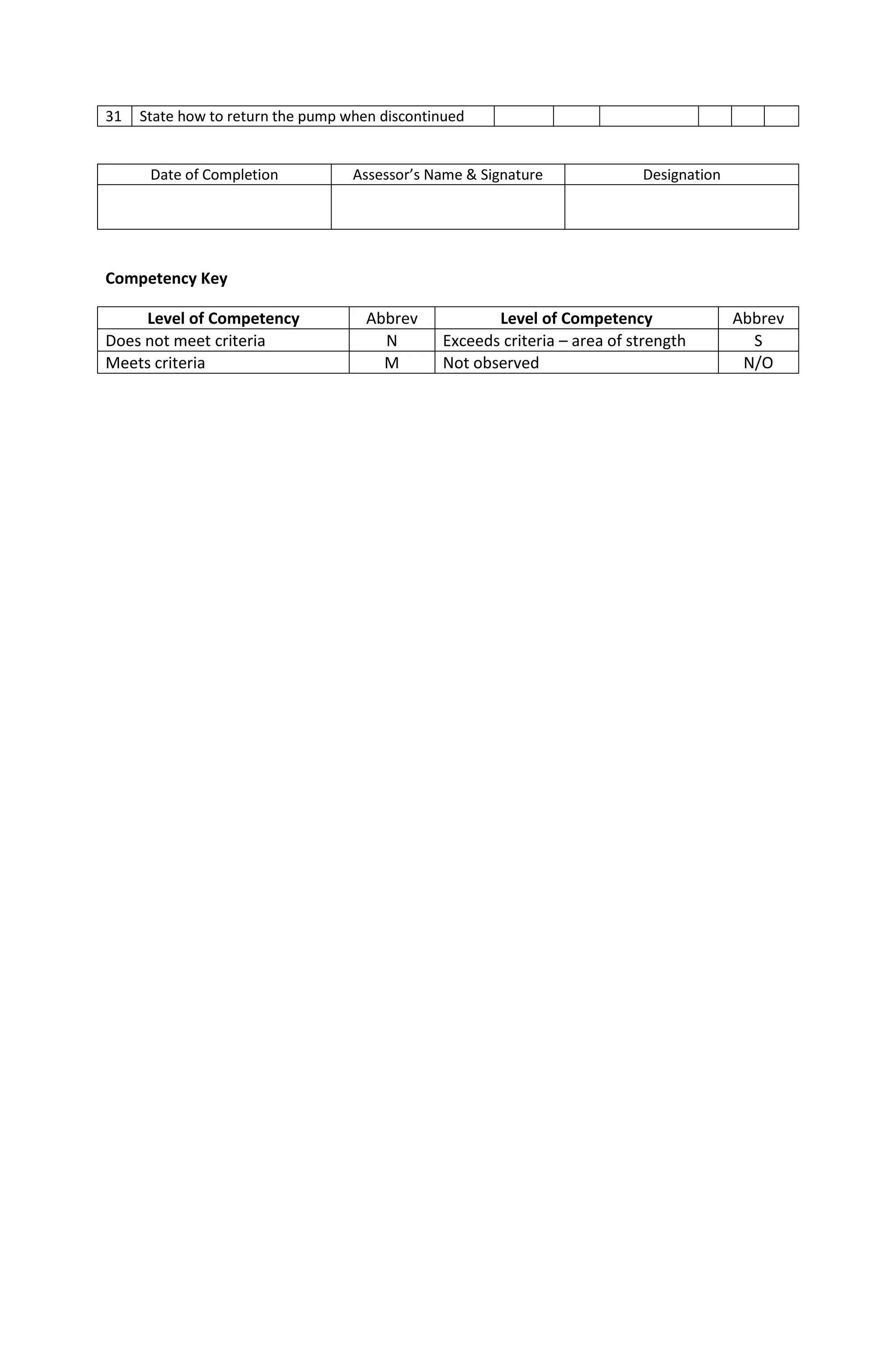
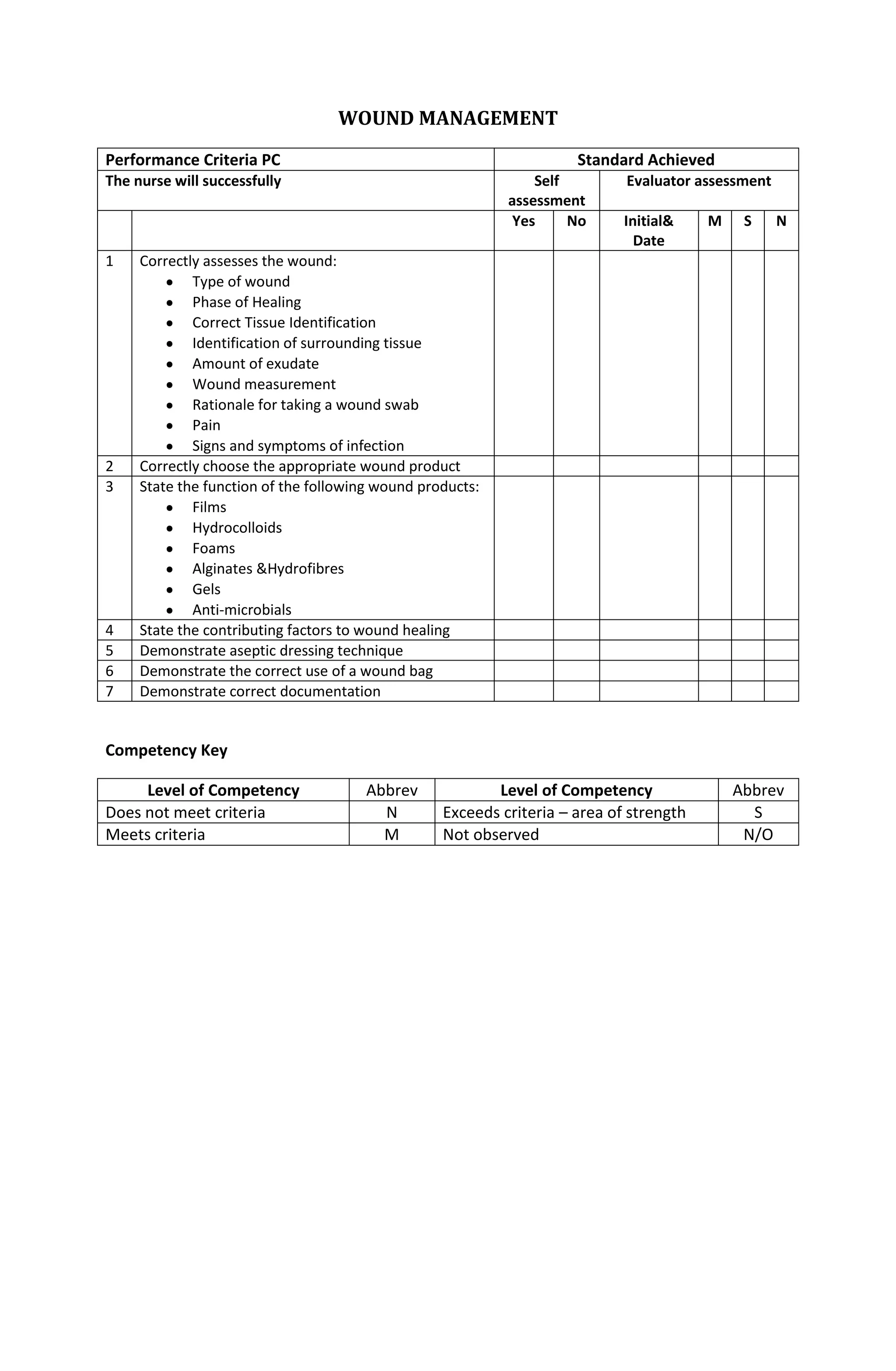
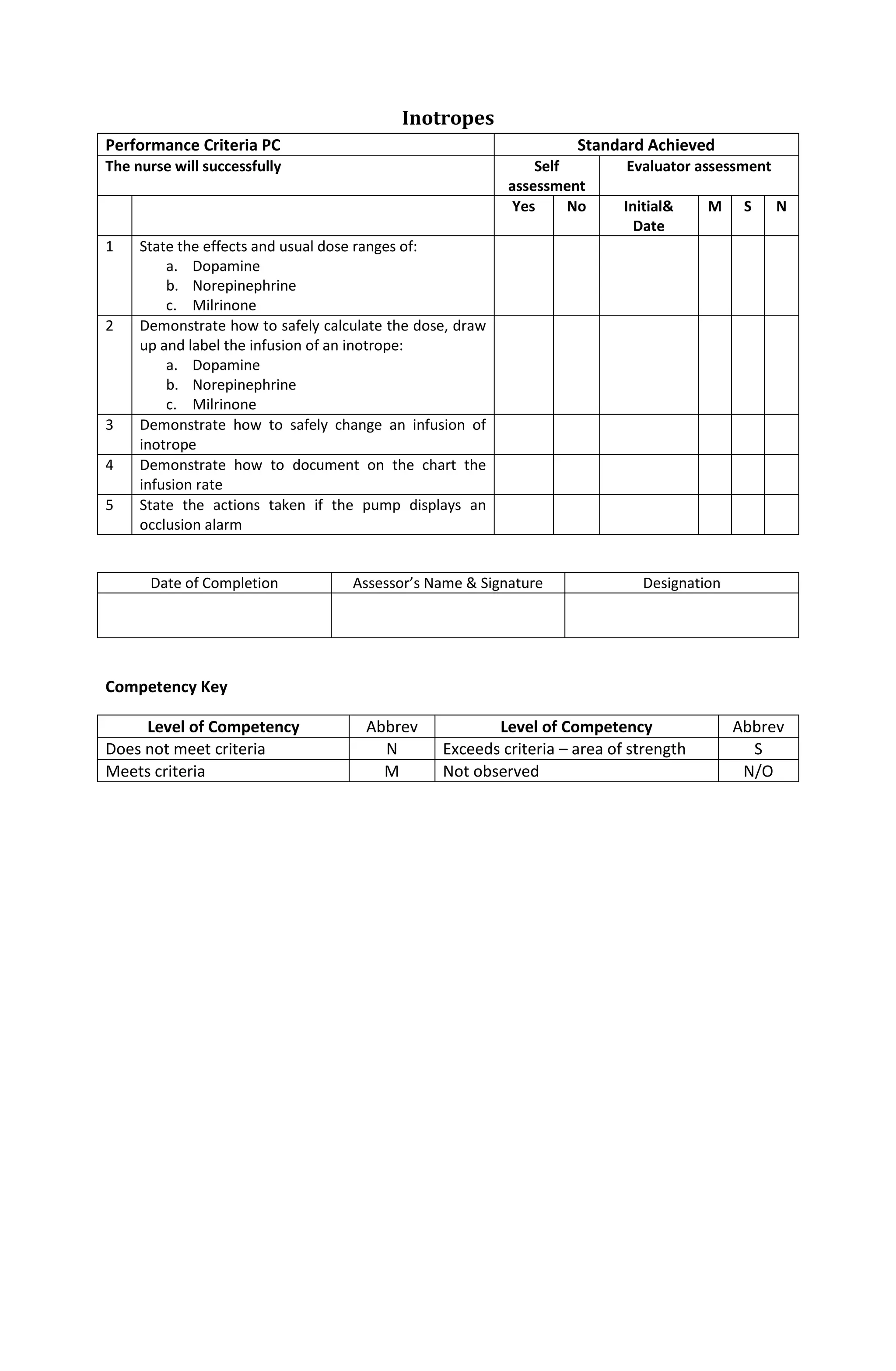
This document contains competency checklists for various critical care nursing skills. It includes skills related to bed safety, bedside equipment, monitoring equipment, infusion devices, ECG rhythm interpretation, airway management, tracheostomies, tissue viability, psychological care of patients, care of dying patients, patient transport, central venous lines, and chest drains. For each skill, the nurse's self-assessment and evaluator's assessment of whether the criteria were met is documented.