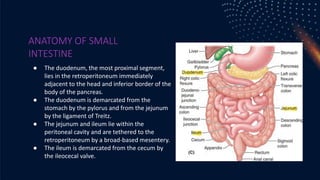
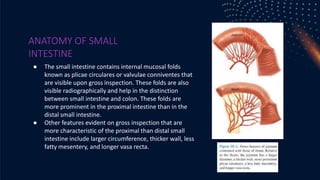
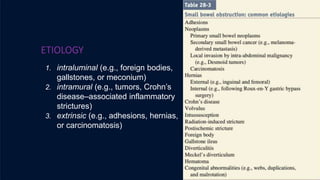
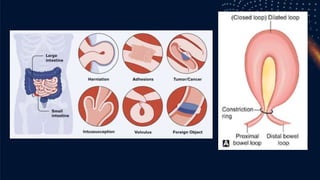
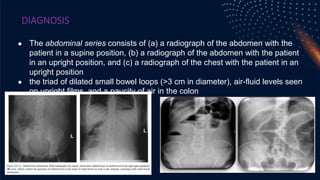
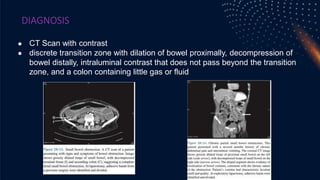
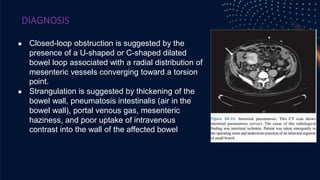
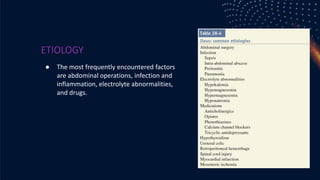
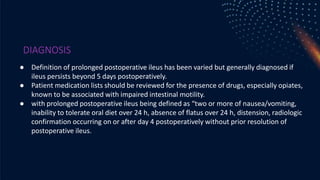
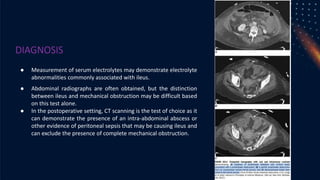
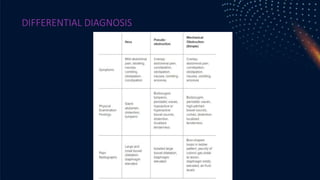
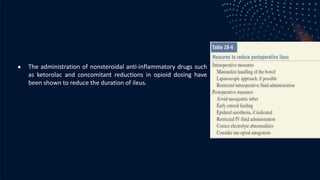
The document provides a comprehensive overview of the anatomy, causes, symptoms, diagnosis, and treatment of small intestine obstruction and postoperative ileus. It emphasizes the importance of understanding the anatomical structure of the small intestine, the types of obstructions, their pathophysiology, clinical manifestations, and diagnostic methods, particularly imaging techniques. Treatment options vary based on the etiology of the obstruction and include surgical intervention, fluid resuscitation, and nutritional support, highlighting the significance of prompt diagnosis and management to prevent severe complications.