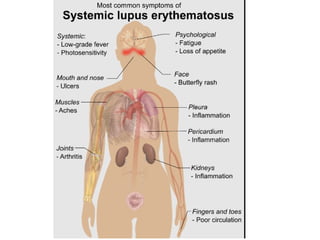
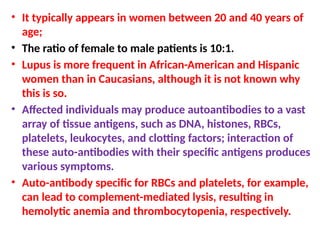
Systemic lupus erythematosus (SLE) is an autoimmune disease where the immune system attacks healthy tissue, presenting symptoms like joint pain, fever, and a facial rash. Predominantly affecting women aged 20-40, its diagnosis relies on specific antinuclear antibodies and various blood tests, while treatment for severe cases includes corticosteroids and immunosuppressants. The disease often leads to complications like vasculitis and glomerulonephritis due to immune complex deposition in small blood vessels.