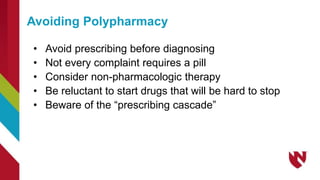
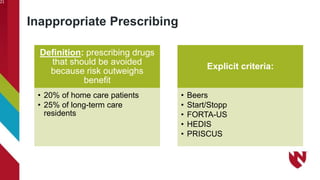
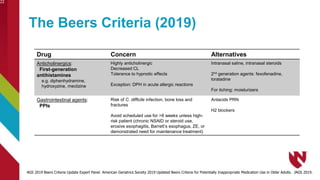
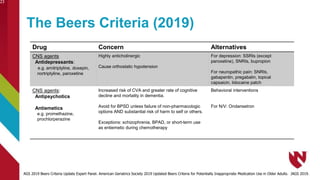
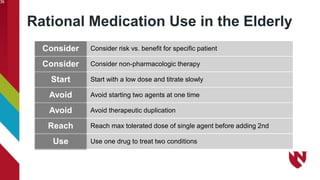
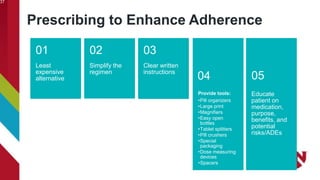
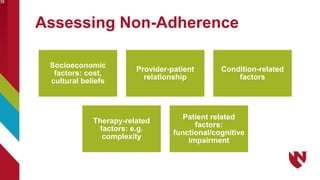
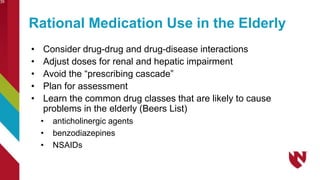
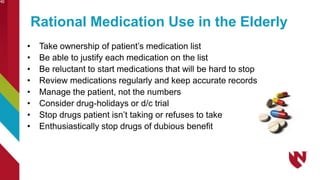
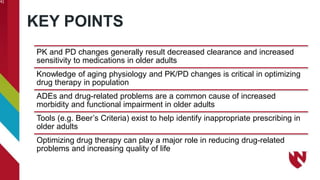
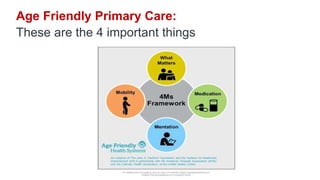
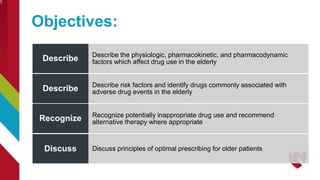
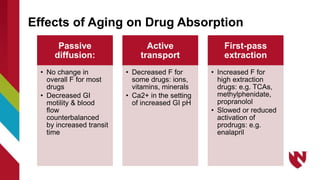
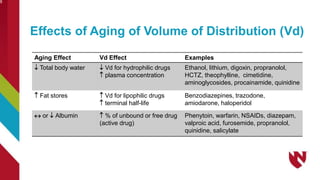
This document provides information about the Nebraska Geriatrics Workforce Enhancement Program (NGWEP). It is a partnership between Nebraska Medicine, UNMC, community organizations, and primary care sites supported by funding from HRSA. The program focuses on age-friendly primary care and improving care for older adults, with a focus on optimizing medication use (the 4Ms) in older patients. The document includes objectives about understanding changes in aging physiology that impact drug use in seniors and identifying risks of polypharmacy and inappropriate prescribing. It also provides guidance on prescribing principles for older adults.


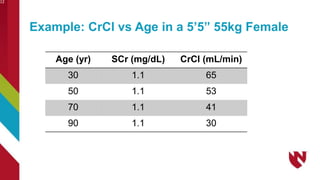
![• SCr alone not a reliable indicator of renal function
• Lean body mass = lower creatinine production
• SCr stays in normal range masking changes in CrCl
• CrCl (Cockroft-Gault) has best predictability in elderly
• CrCl =
Estimating GFR in the Elderly
(ABW in kg) x (140-age)
------------------------------ x (0.85 for females)
72 x (Scr in mg/dL)
Use adjusted body weight (AjBW) if BMI >40 kg/m2
BMI = ABW in kg/[ht in meters]2 OR 703 x (WT (lbs)/[HT (in)]2)](https://image.slidesharecdn.com/4msmedicationsobeski071922-240203115227-ebee126d/85/4Ms_Medication_Sobeski_071922-pptx-11-320.jpg)