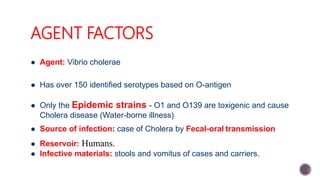
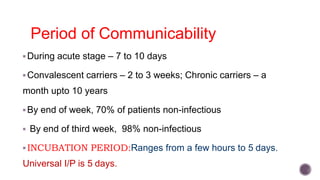
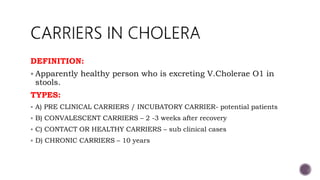
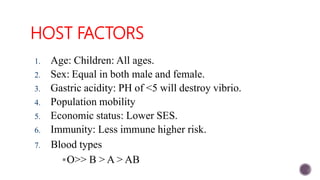
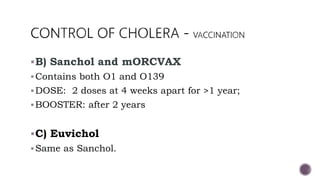
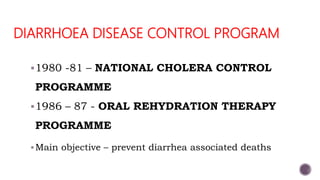
Cholera is an acute diarrheal disease caused by the bacterium Vibrio cholerae O1. It spreads through contaminated food or water and causes profuse watery diarrhea and vomiting that can lead to severe dehydration and death if untreated. The key aspects of cholera prevention and control include early detection and treatment with oral rehydration, antibiotic therapy, improved water and sanitation, vaccination in at-risk areas, and health education on hygiene practices. National programs in India have focused on these measures to reduce the burden of cholera.