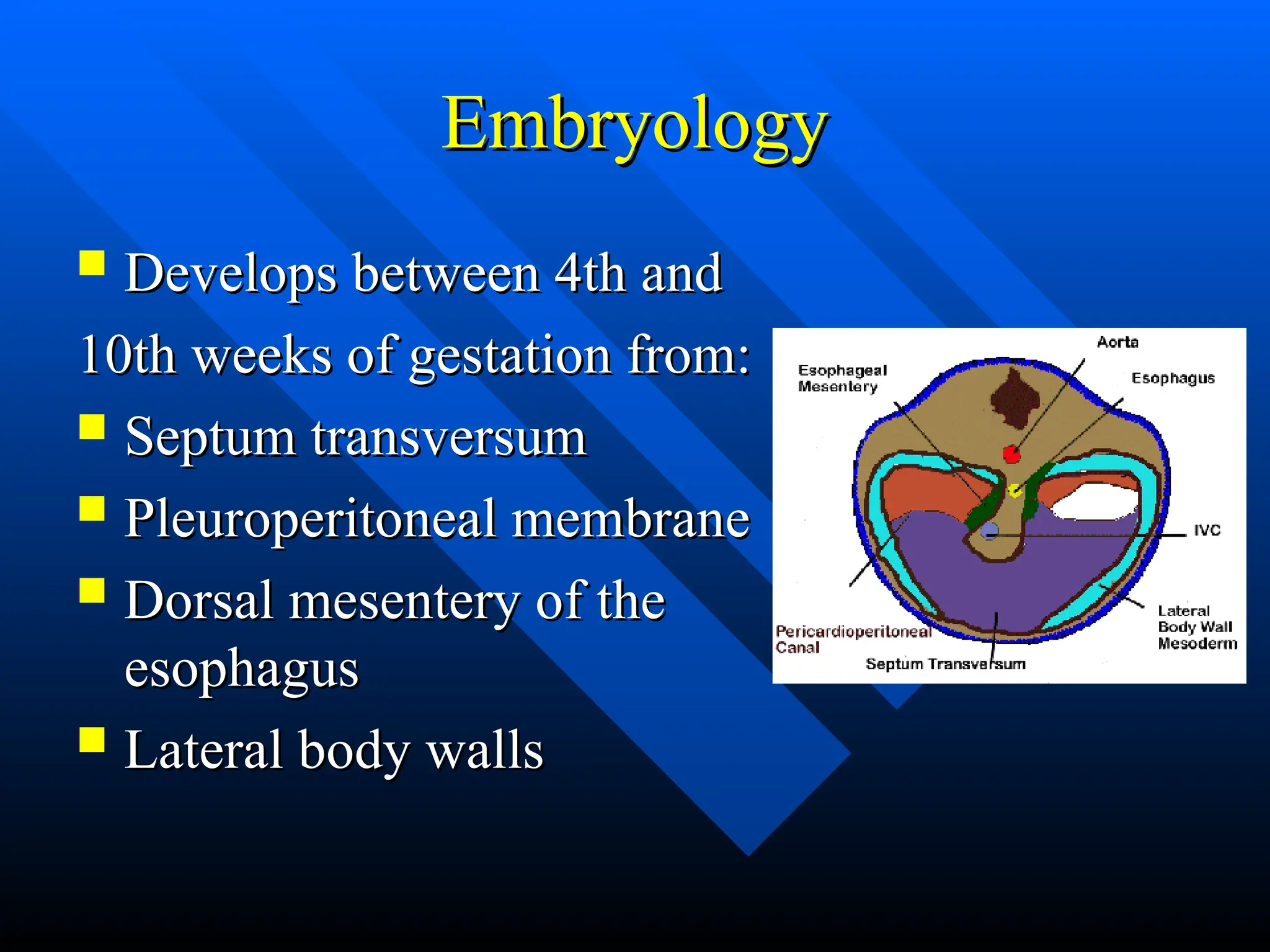
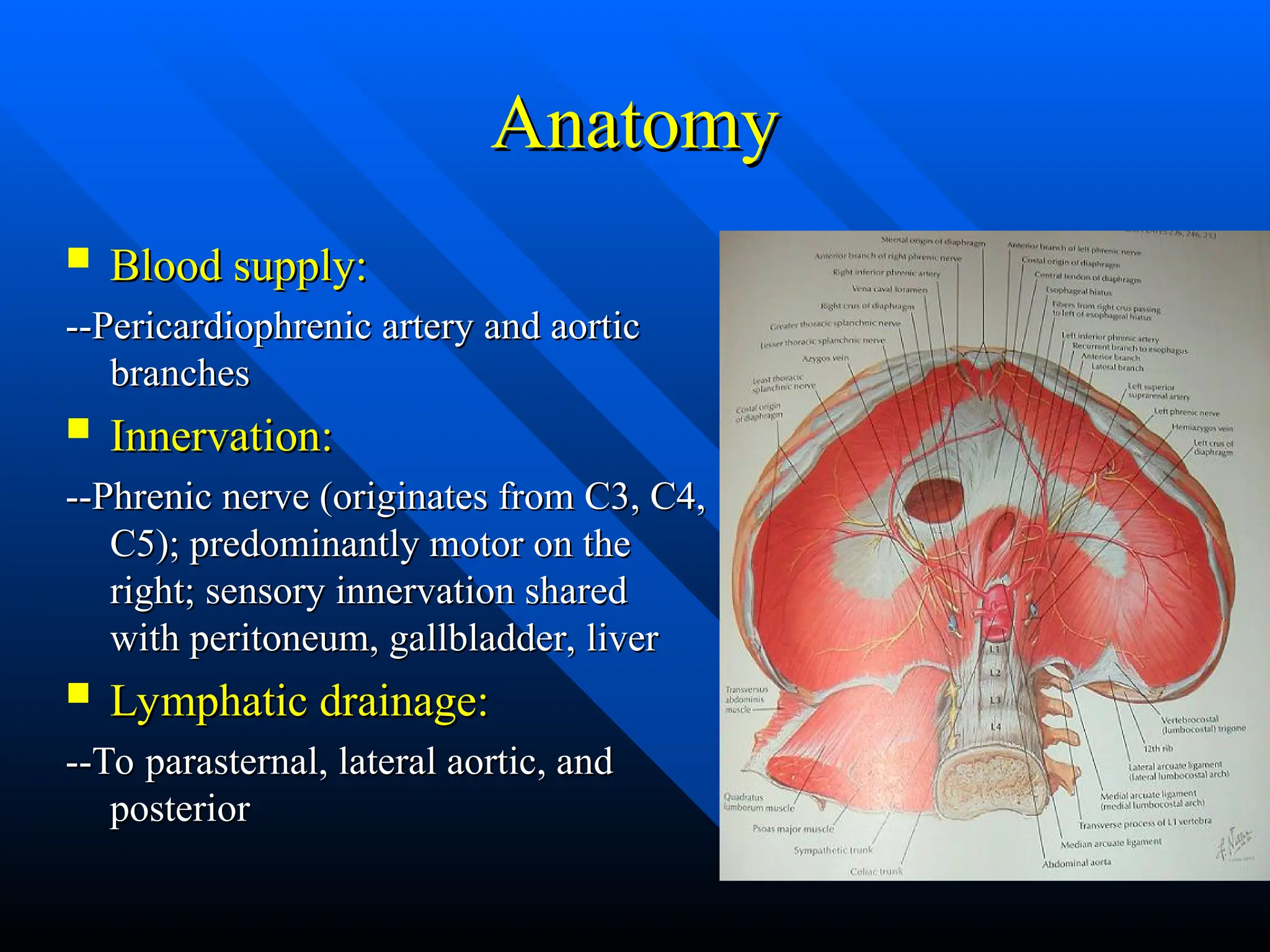
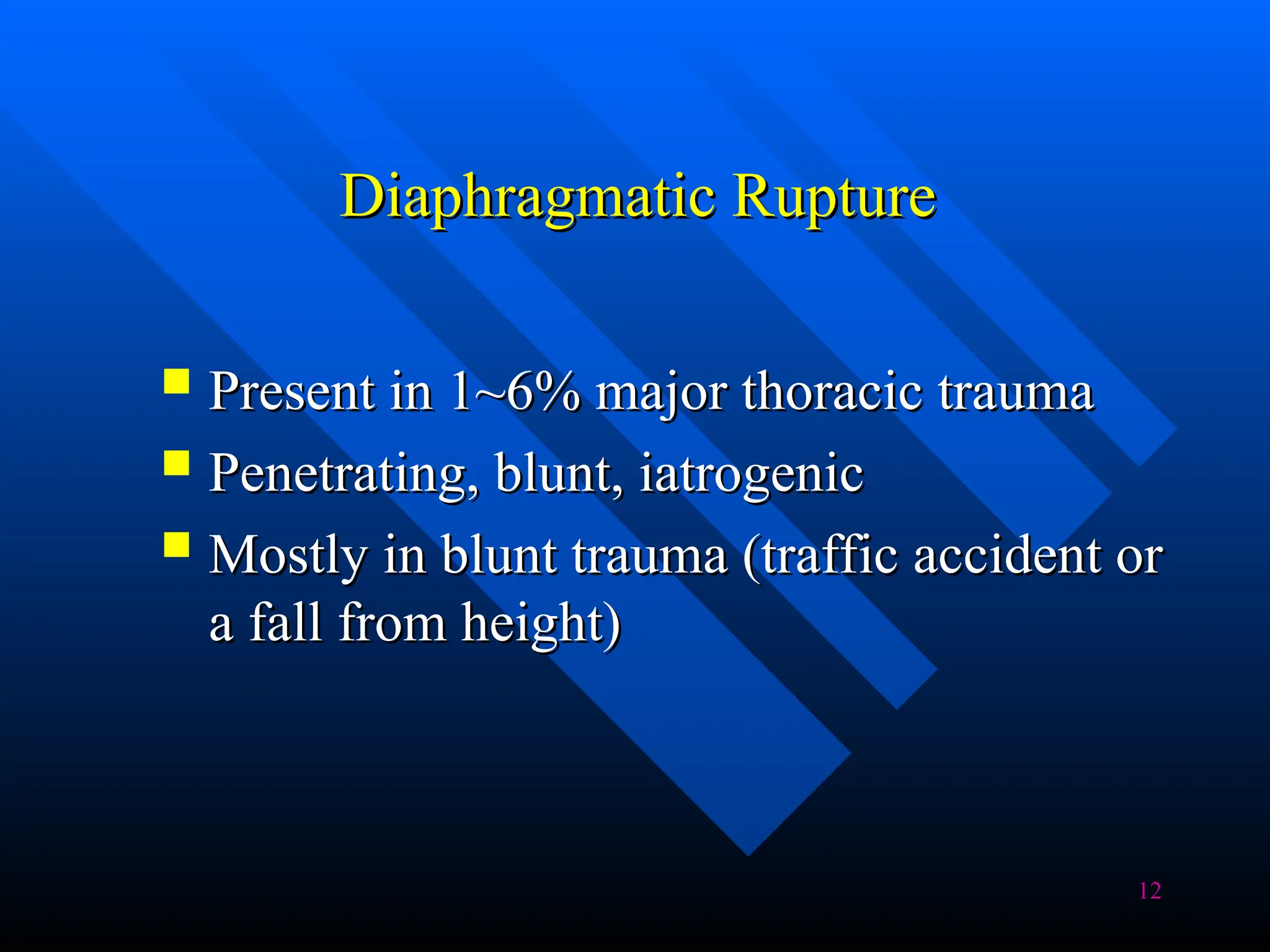
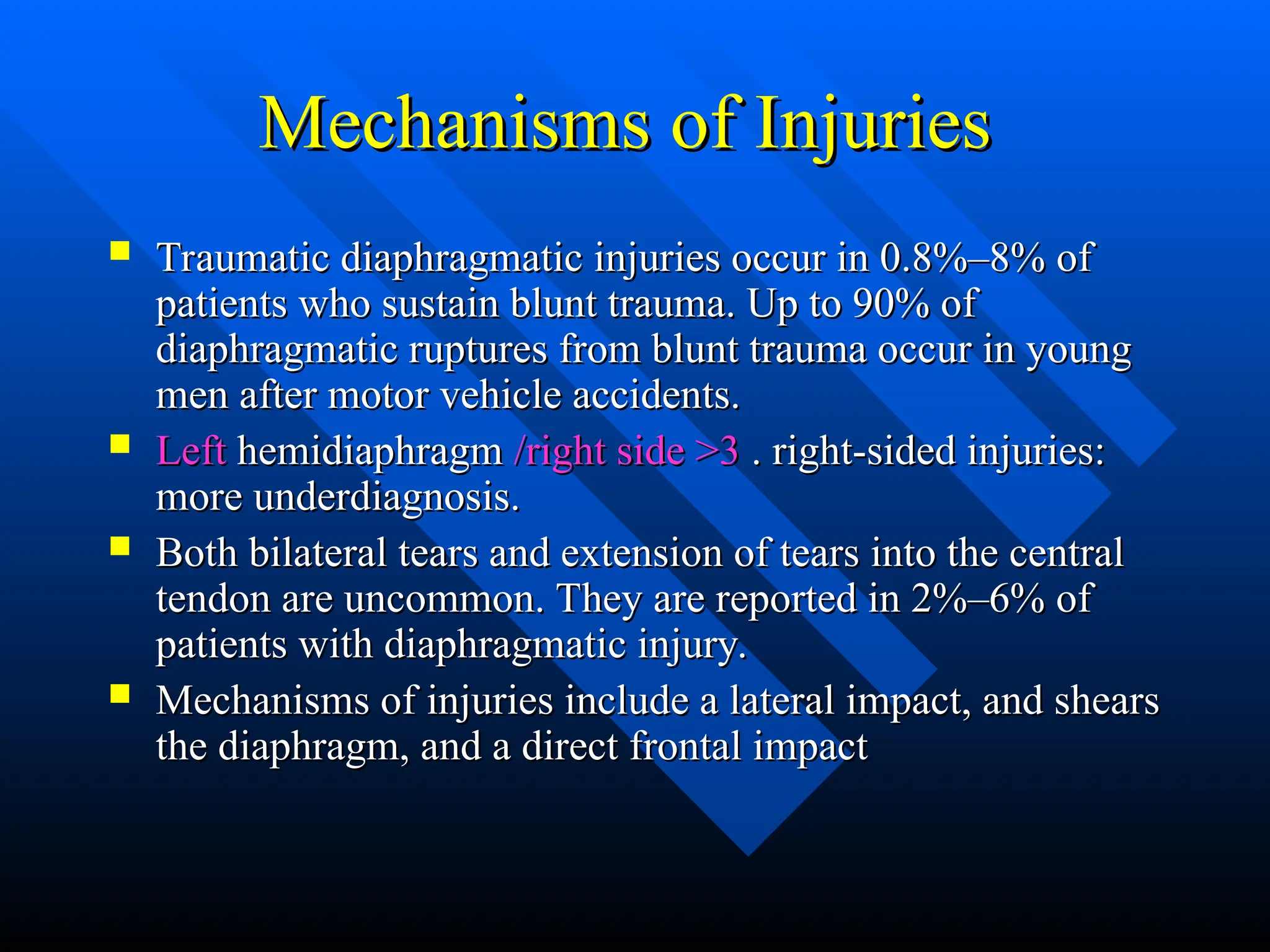
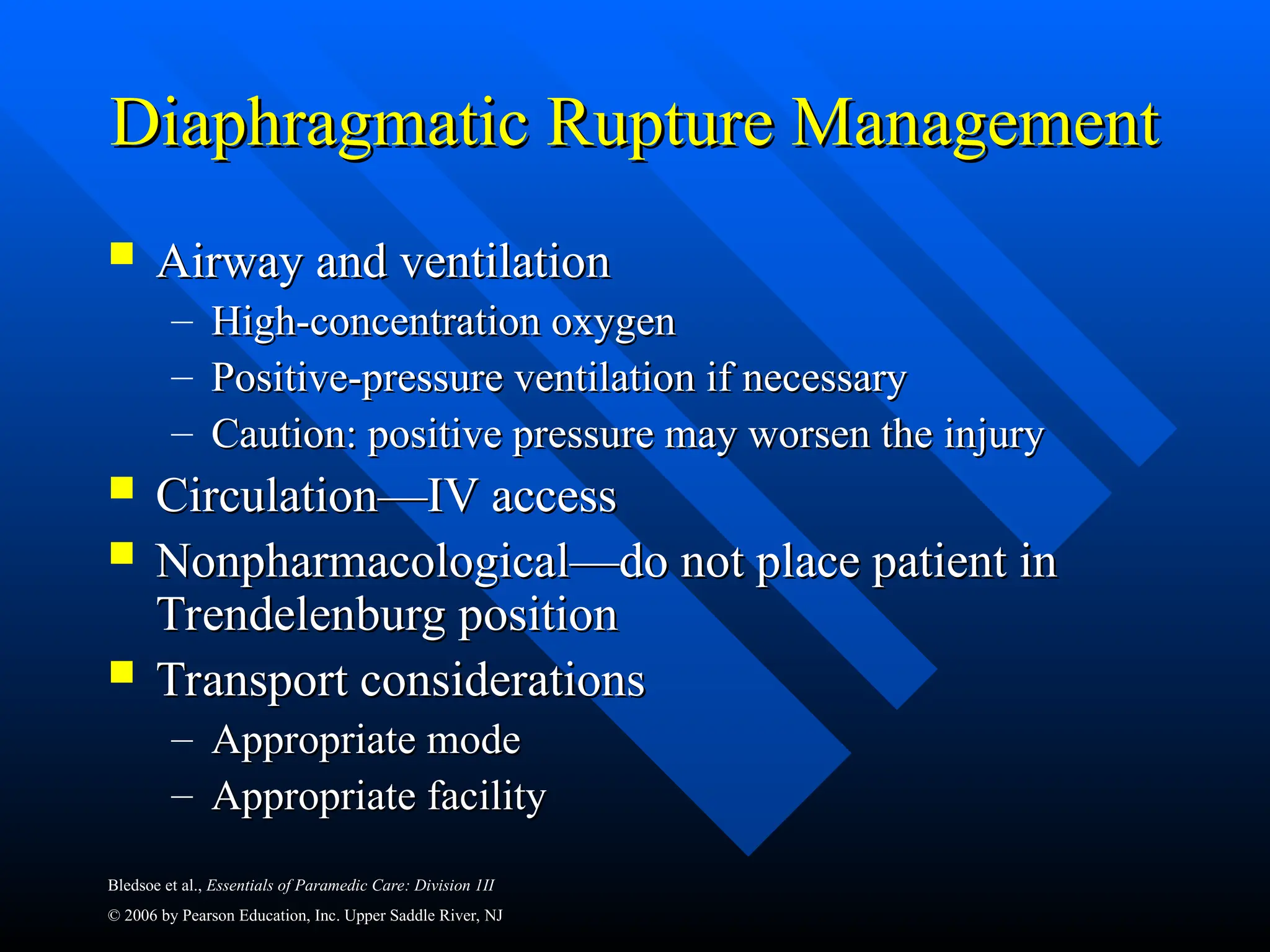
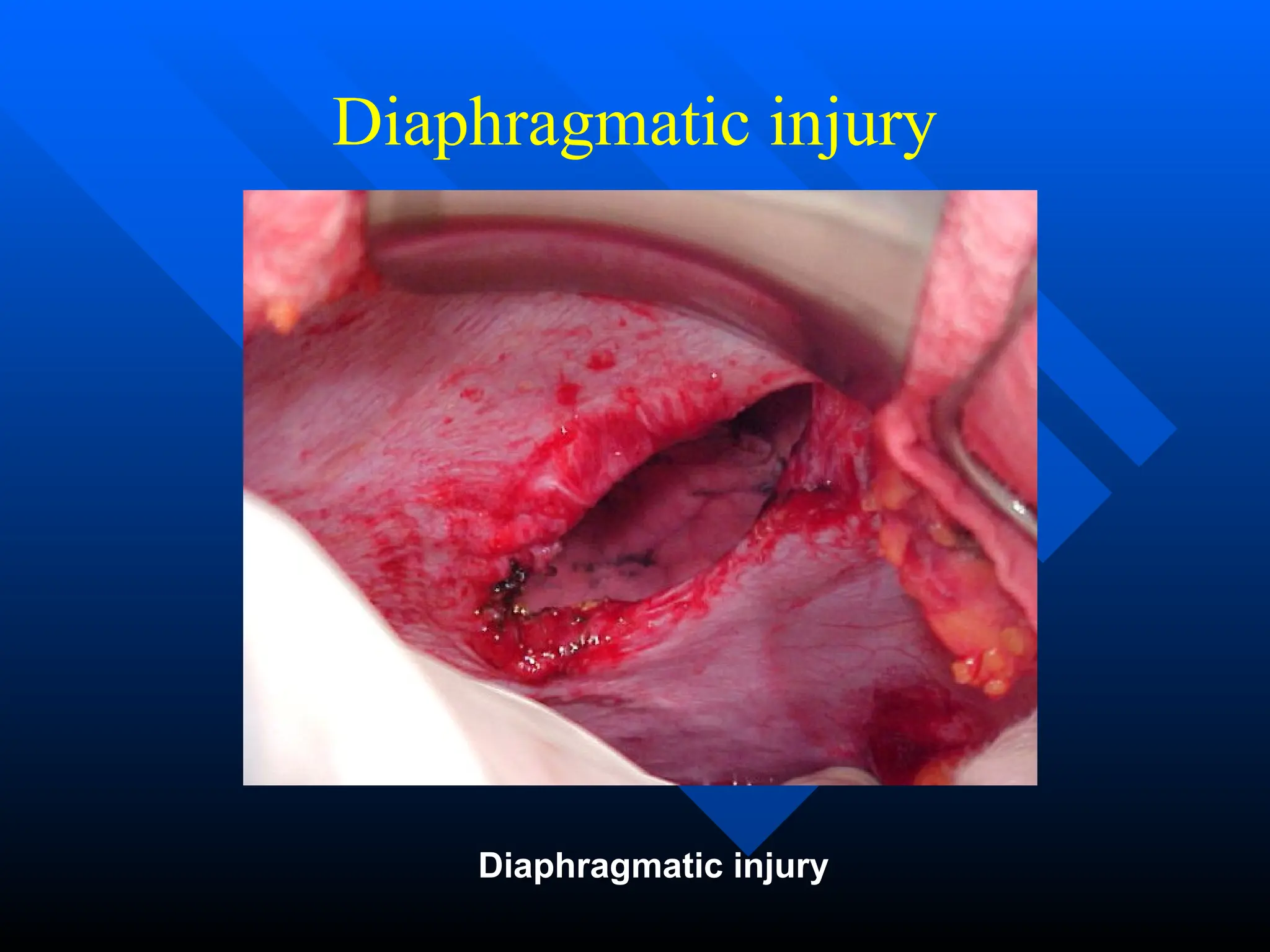
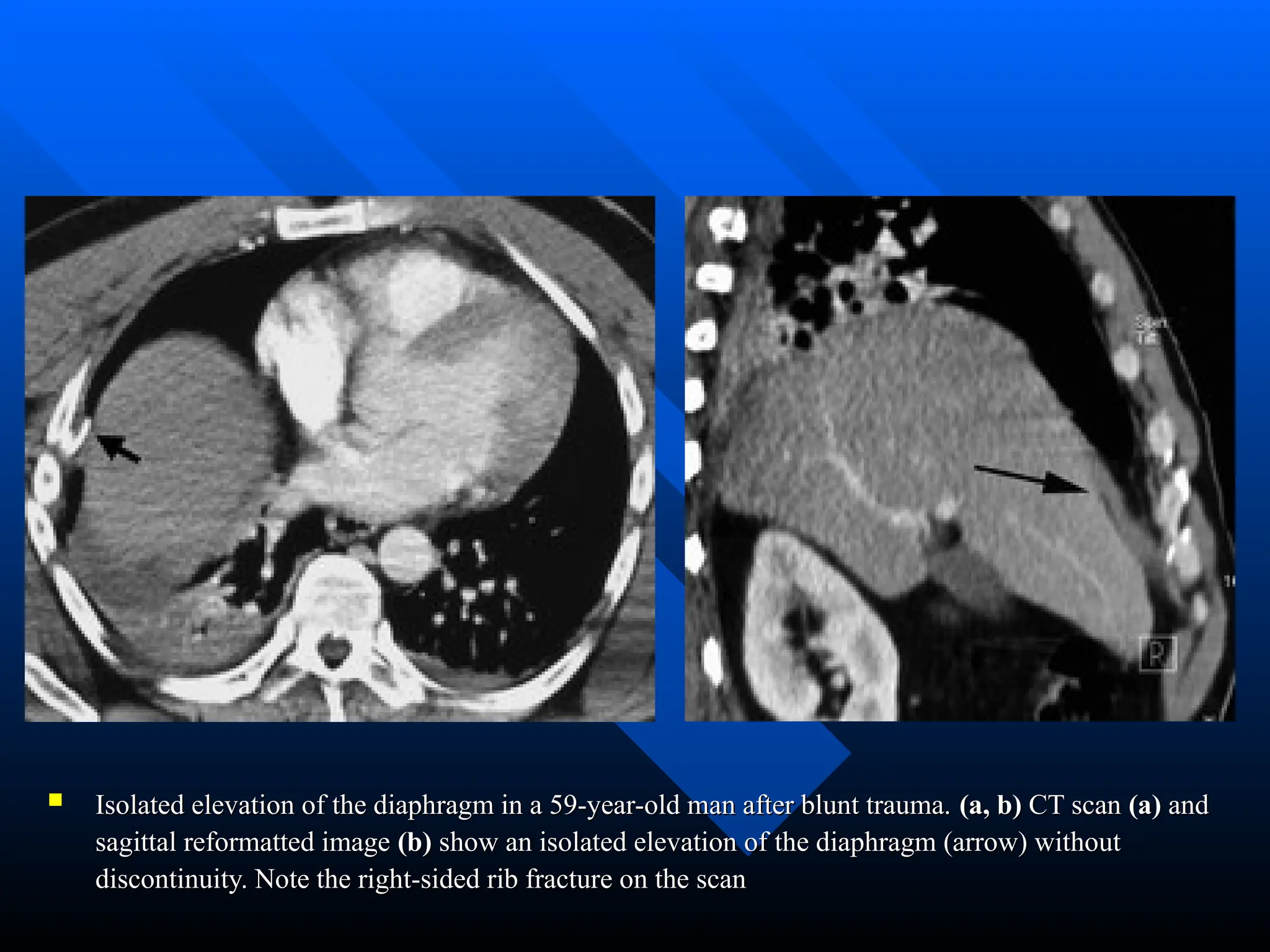
The document discusses diaphragmatic rupture, detailing its embryological development, anatomical components, and clinical implications. It highlights that such ruptures can arise from blunt or penetrating trauma, with a significant occurrence in traffic accidents, and identifies the complications and associated injuries linked to these ruptures. Diagnosis can be challenging, as symptoms may be subtle and patients may present differently based on the phase of the injury.
































![58
Refrences
Diaphragm rupture
Diaphragm rupture
Clinical radiology.61(6):467-77, 2006 Jun.
Clinical radiology.61(6):467-77, 2006 Jun.
Ultrasound detection of right-sided diaphragmatic injury; the
Ultrasound detection of right-sided diaphragmatic injury; the
“liver sliding” sign
“liver sliding” sign
American Journal of Emergency Medicine (2006) 24, 251–257
American Journal of Emergency Medicine (2006) 24, 251–257
Traumatic rupture of the diaphragm: experience with 65
Traumatic rupture of the diaphragm: experience with 65
patients
patients
Injury, Int. J. Care Injured 34 (2003) 169–172
Injury, Int. J. Care Injured 34 (2003) 169–172
Diagnosis of Blunt Rupture of the Right Hemidiaphragm by
Diagnosis of Blunt Rupture of the Right Hemidiaphragm by
Technetium Scan
Technetium Scan
The American Surgeon [Am Surg], 1999 Aug; Vol. 65 (8), pp. 761-5
The American Surgeon [Am Surg], 1999 Aug; Vol. 65 (8), pp. 761-5](https://image.slidesharecdn.com/diaphragmaticrupturethelect-250129133407-45553681/75/Diaphragmatic-rupture-injuries-how-to-repair-the-lect-ppt-58-2048.jpg)
