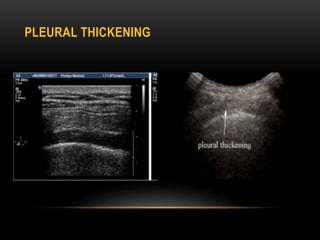
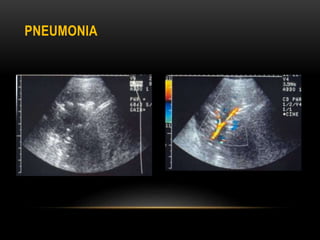
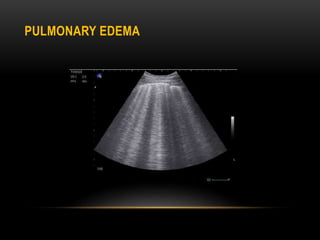
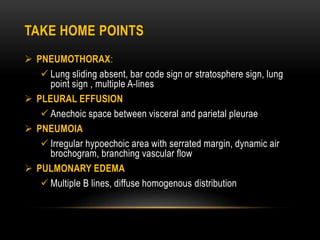
This document provides an overview of chest ultrasound, including the sonographic anatomy, instrumentation, techniques, pathologies, and limitations. It discusses how chest ultrasound can be used to assess pulmonary, pleural, and chest wall lesions. Key findings are described for pneumothorax, pleural effusion, pneumonia, pulmonary edema, and pulmonary masses. The document emphasizes that chest ultrasound is useful for evaluating pleural effusions, pneumothorax, and guiding procedures, but its value in directly evaluating lung tissue remains limited due to artifacts.