The document discusses various topics related to chemotherapy in infectious diseases including:
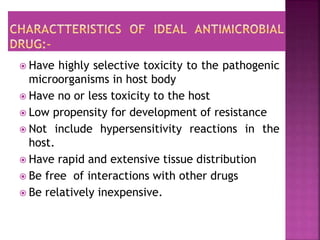
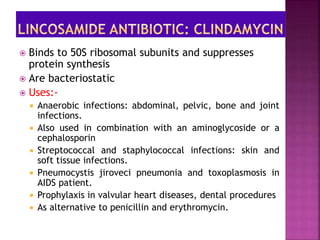
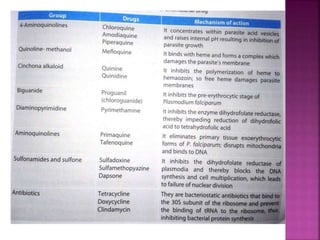
1. It defines chemotherapy as using chemicals to treat diseases caused by microorganisms. Antimicrobials kill or inhibit microorganism growth.
2. Antibiotics are a type of antimicrobial but not all antimicrobials are antibiotics. The first antibiotic, penicillin, was discovered by Alexander Fleming.
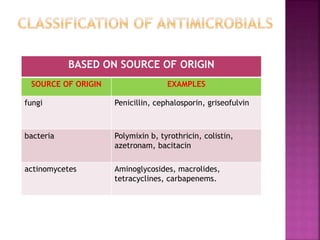
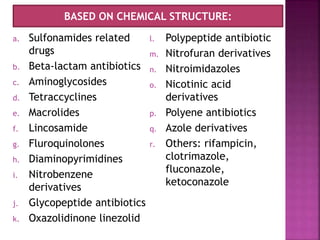
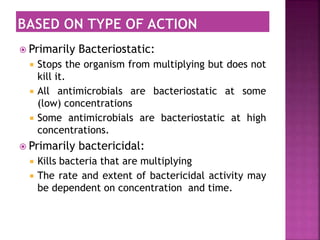
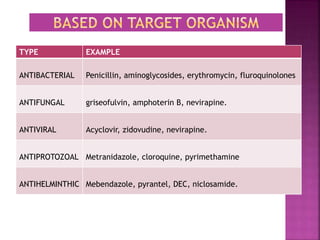
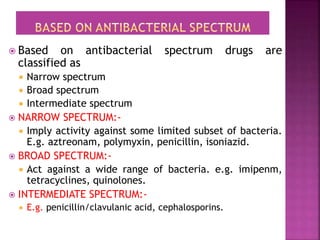
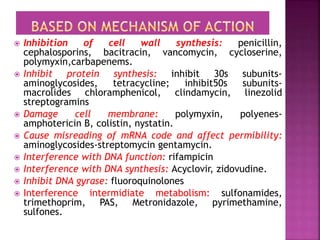
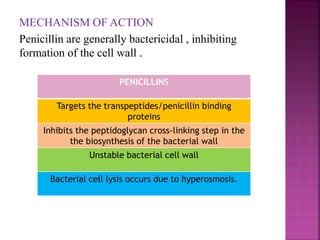
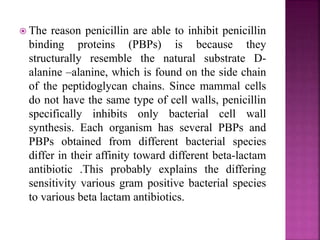
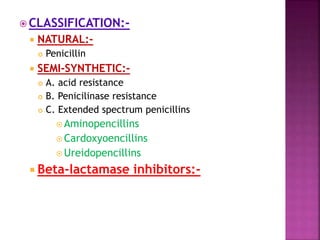
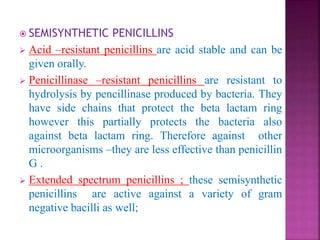
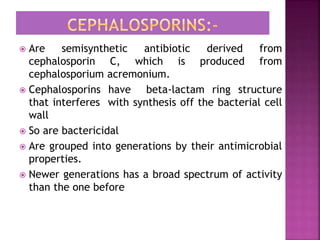
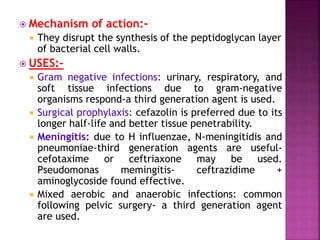
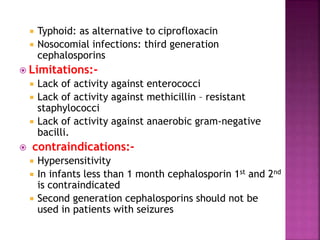
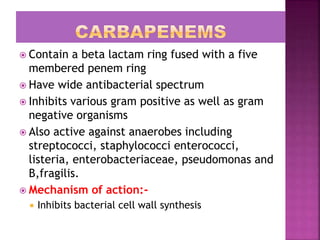
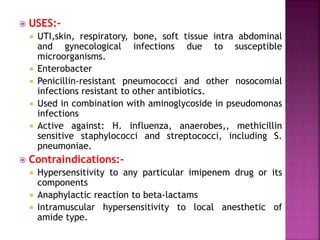
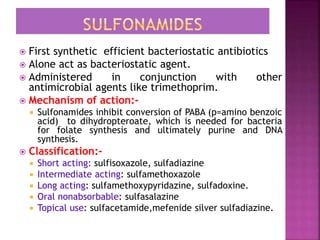
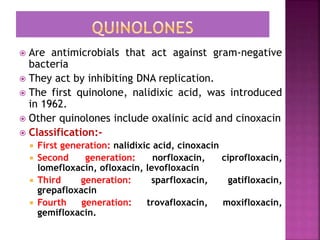
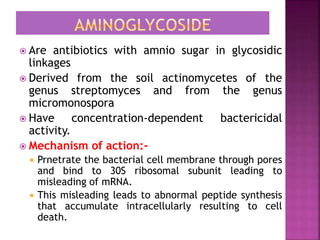
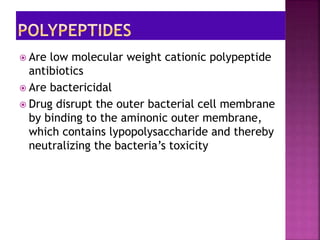
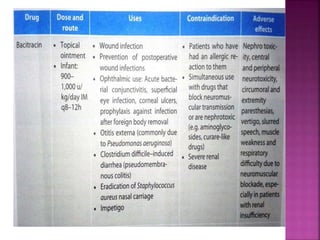
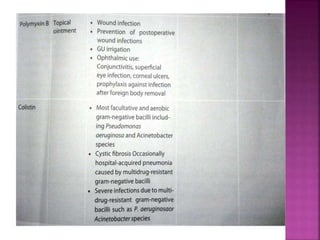
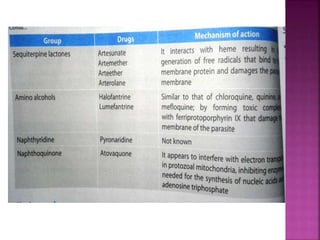
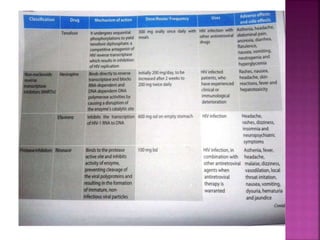
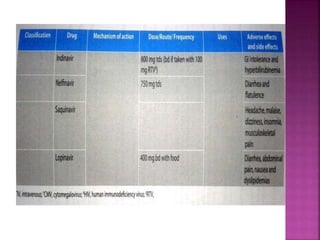
3. Antimicrobials can be classified based on their source, chemical structure, mechanism of action, and spectrum of activity.
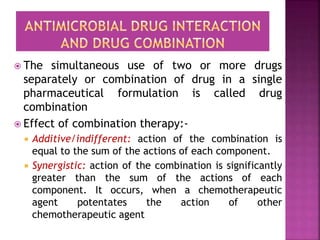
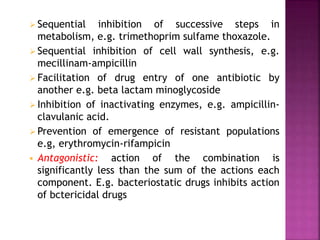
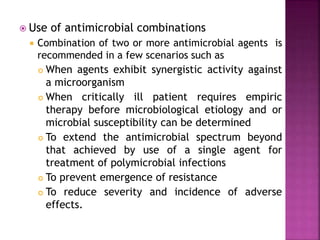
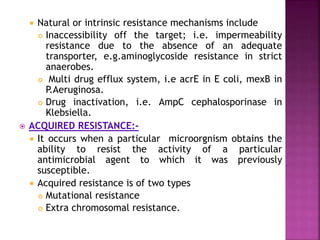
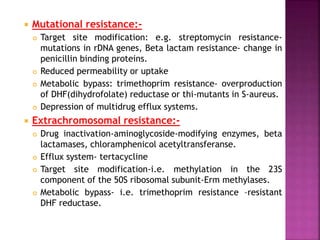
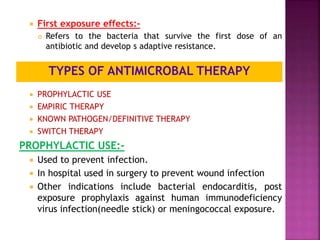
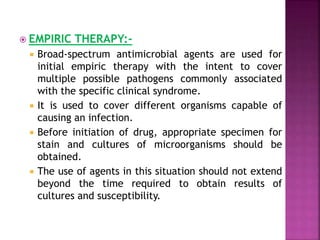
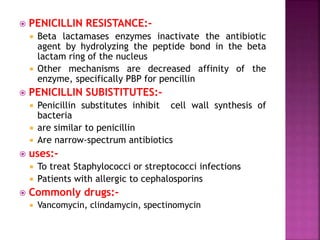
4. Combination antimicrobial therapy and issues of antimicrobial resistance are also discussed.