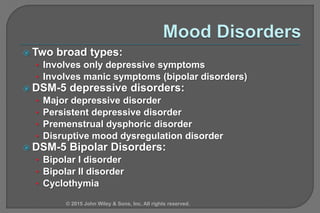
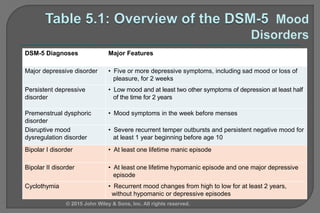
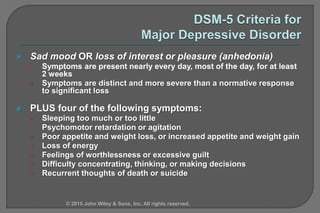
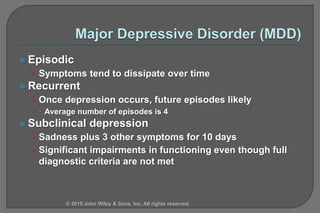
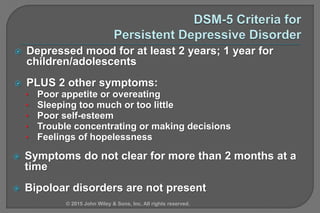
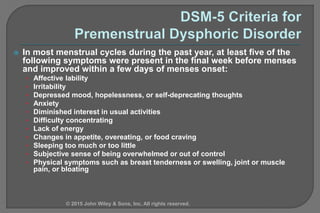
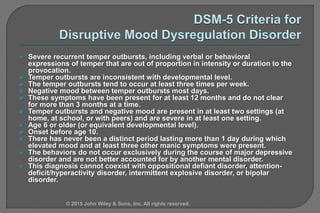
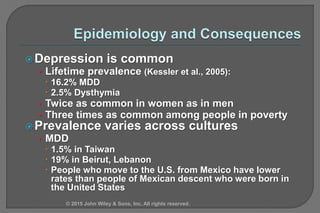
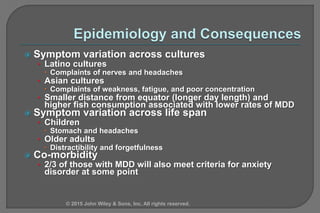
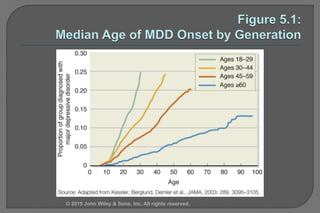
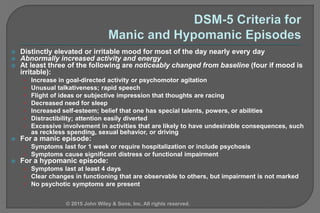
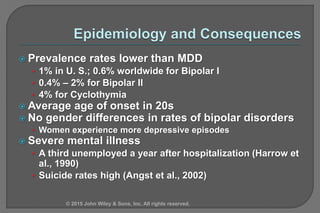
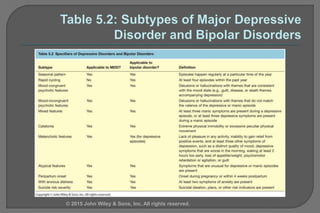
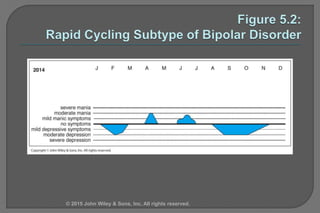
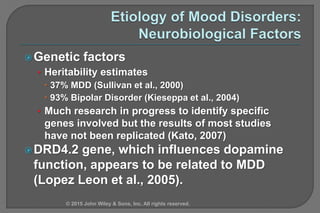
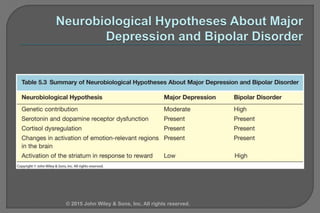
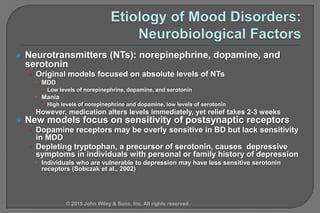
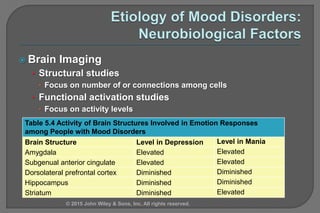
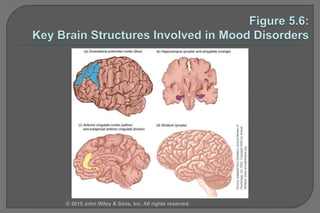
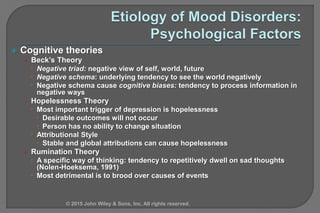
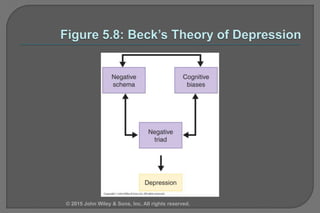
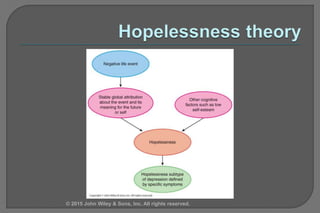
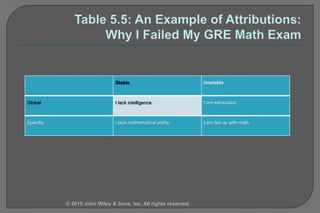
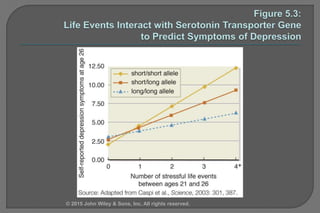
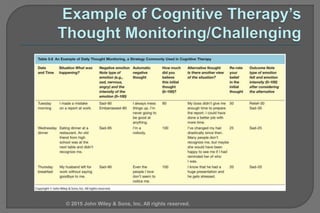
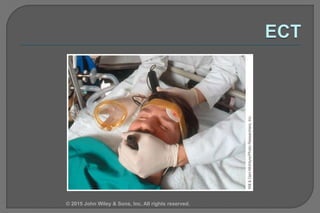
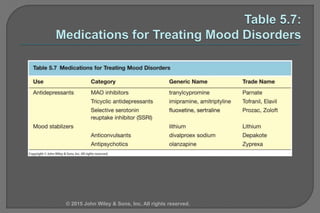
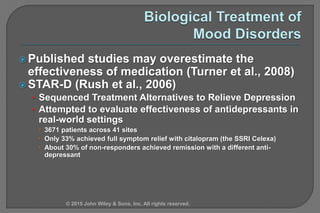
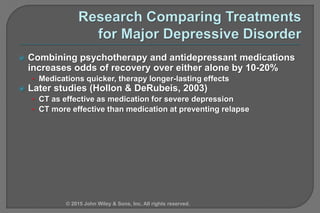
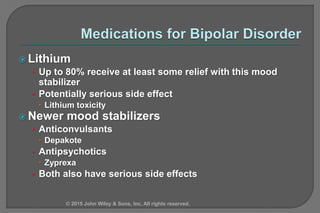
The document provides an overview of mood disorders, including their classifications such as major depressive disorder, persistent depressive disorder, and bipolar disorders. It discusses the clinical descriptions, epidemiology, etiology, treatment options, and the prevalence of these disorders, highlighting the impact of genetics, neurotransmitter levels, and psychosocial factors. Additionally, it covers various therapeutic approaches and the effectiveness of medication and psychotherapy in treating mood disorders.