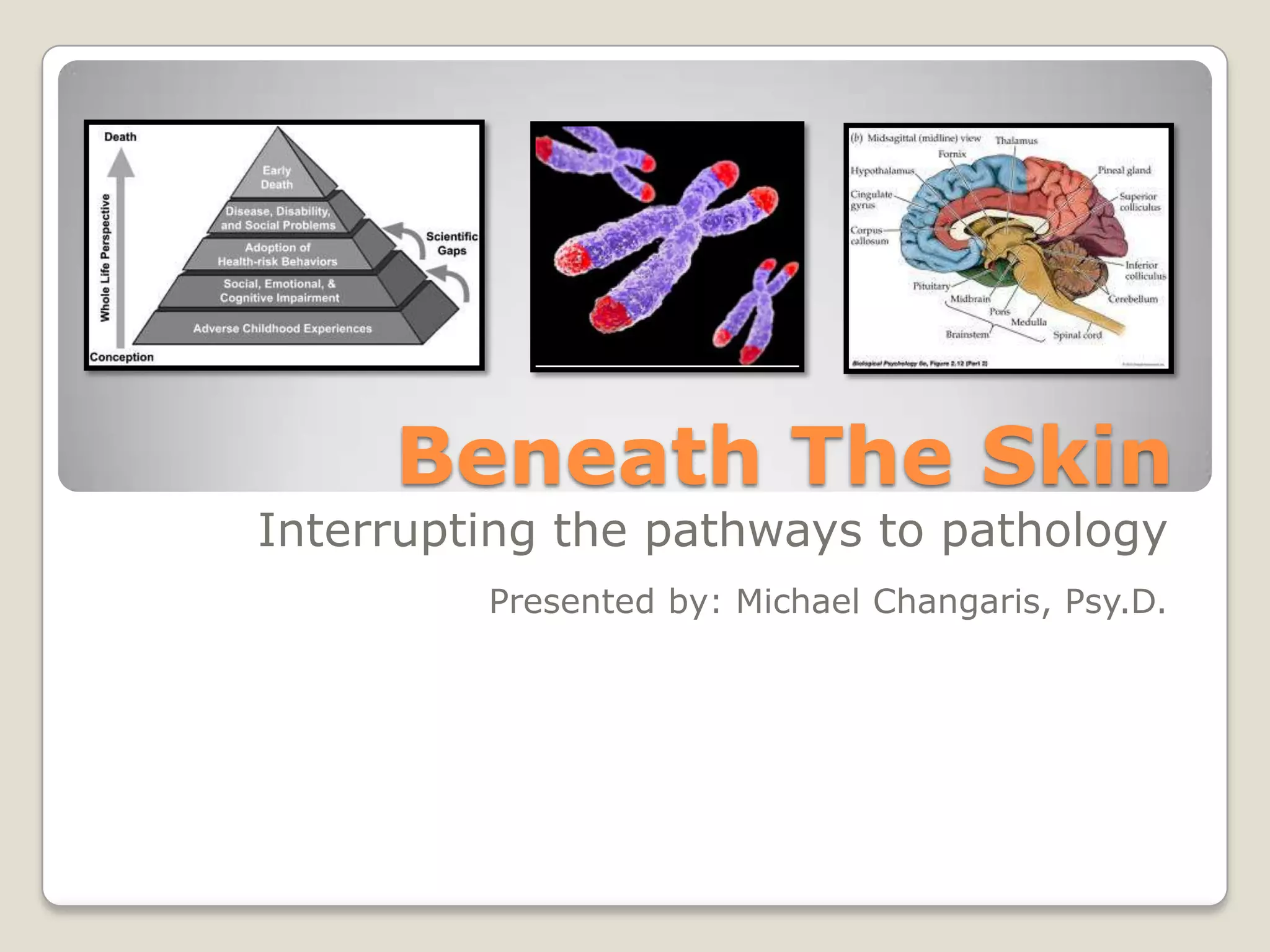
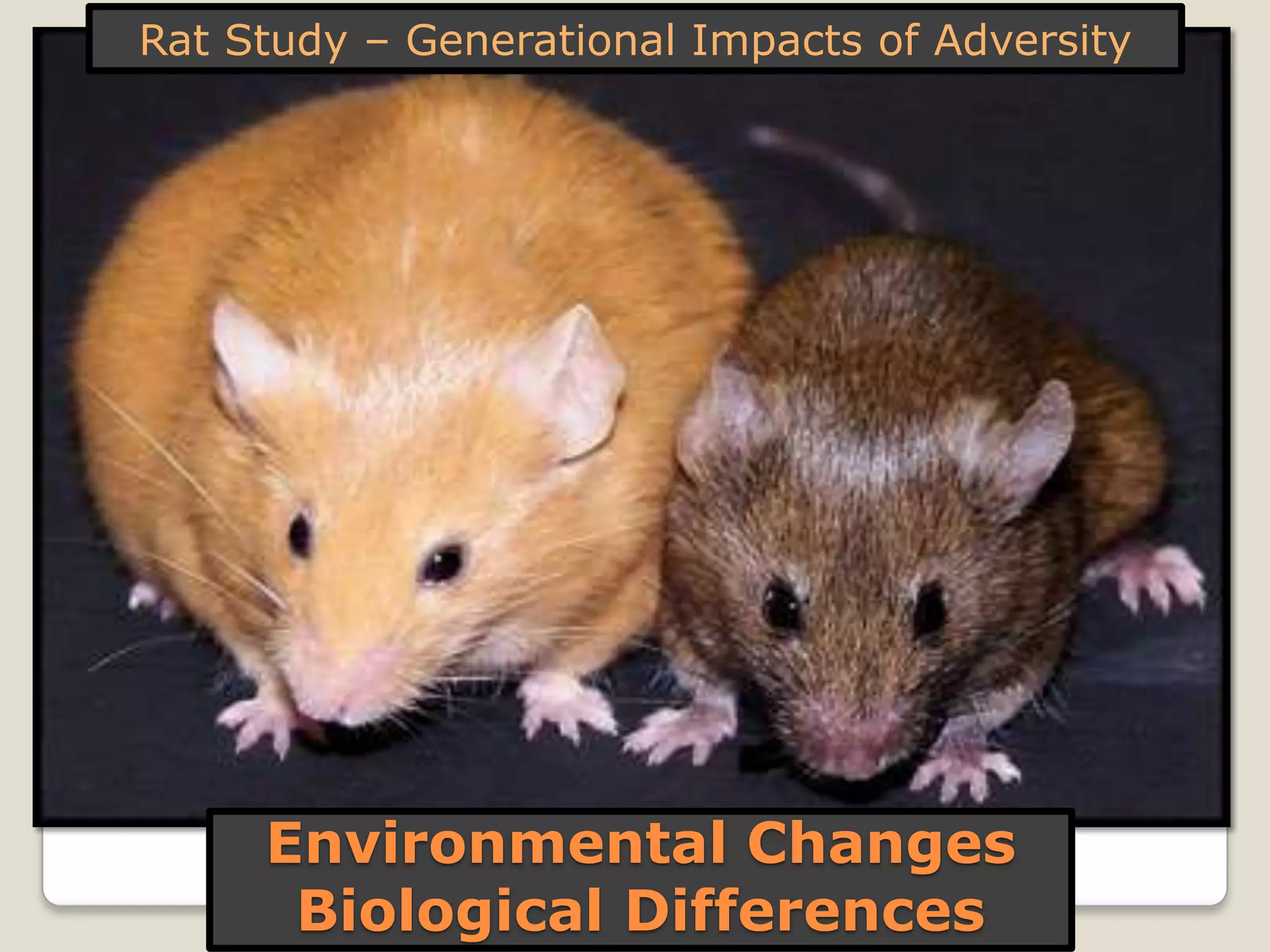
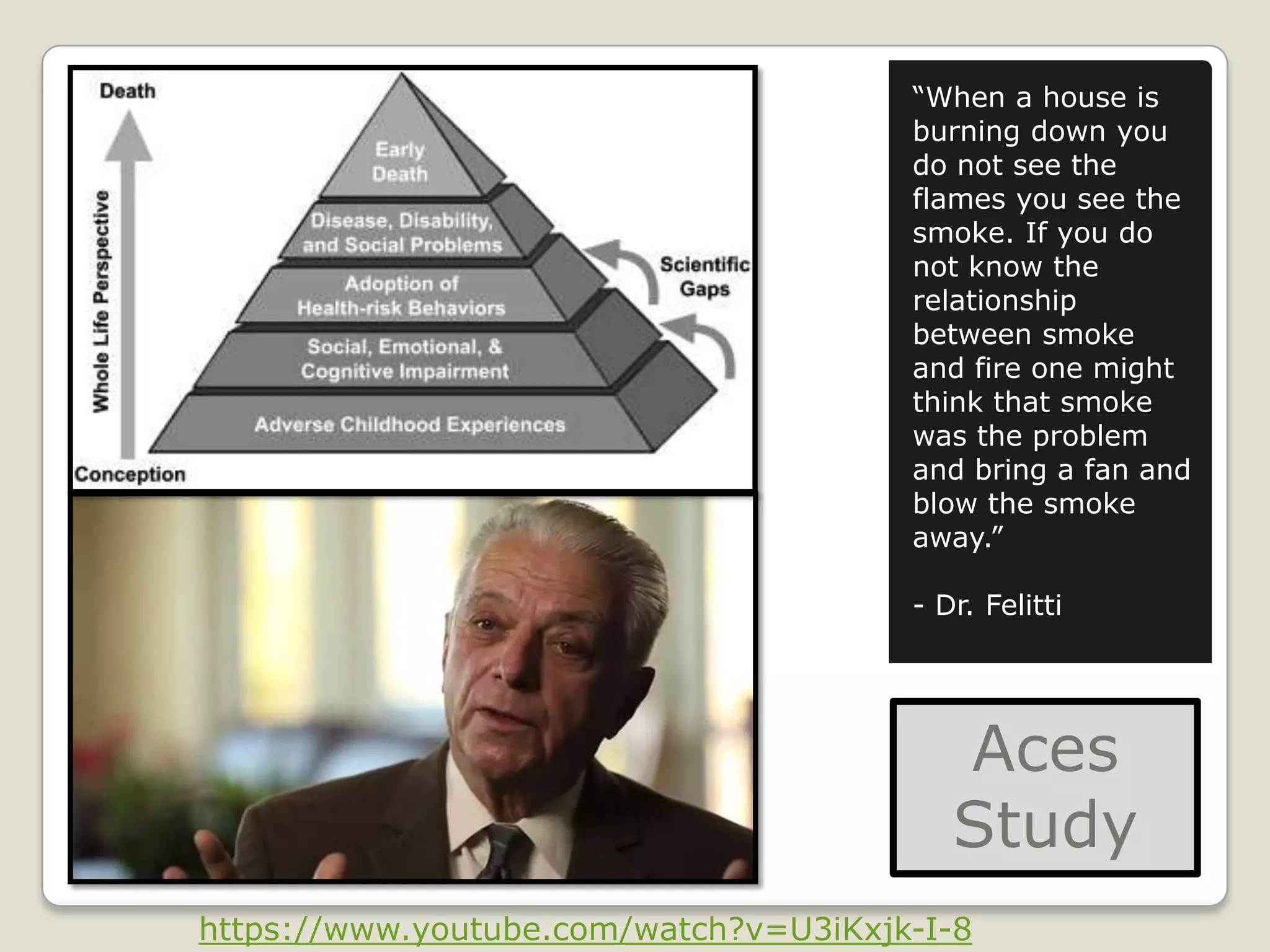
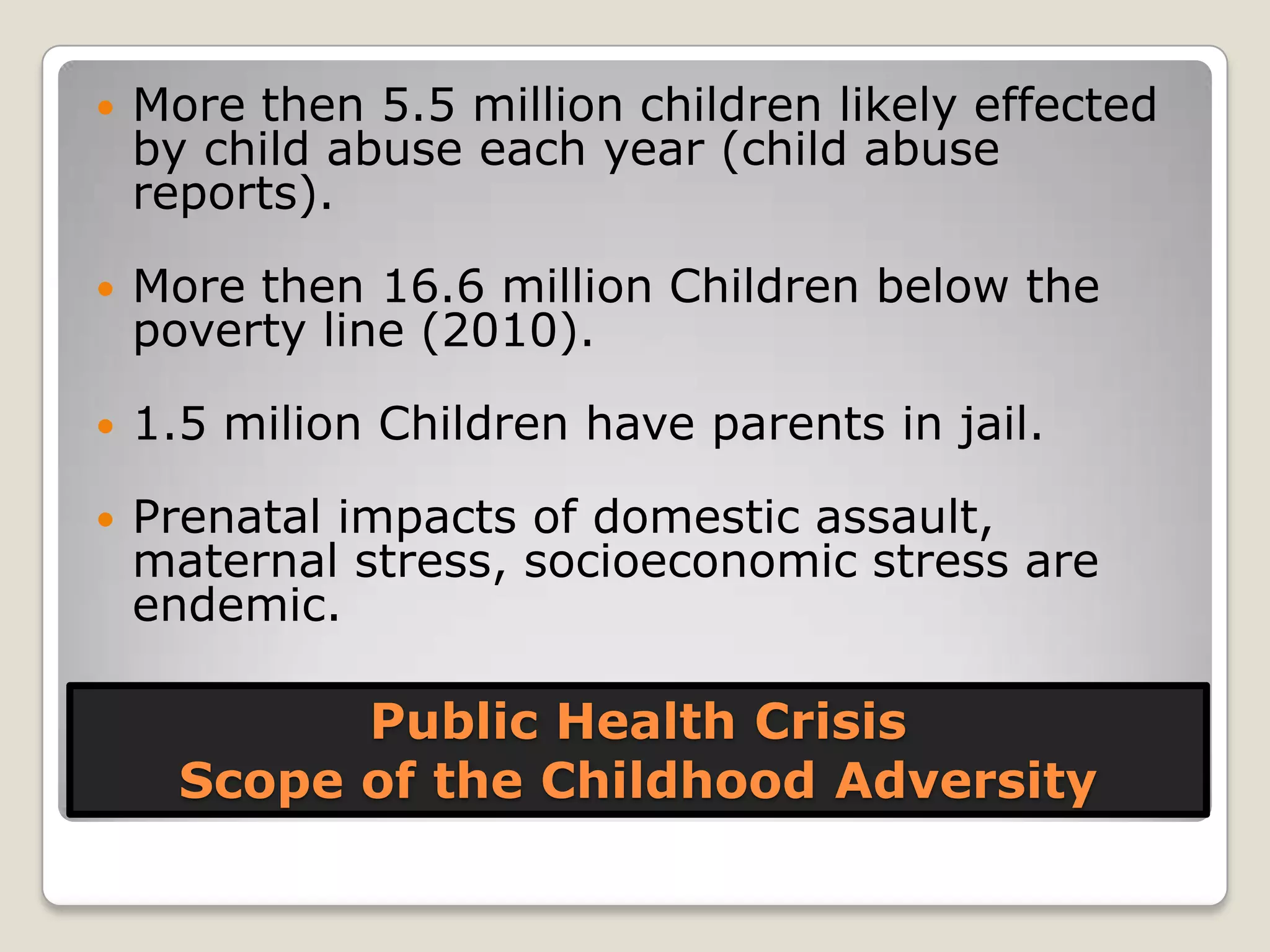
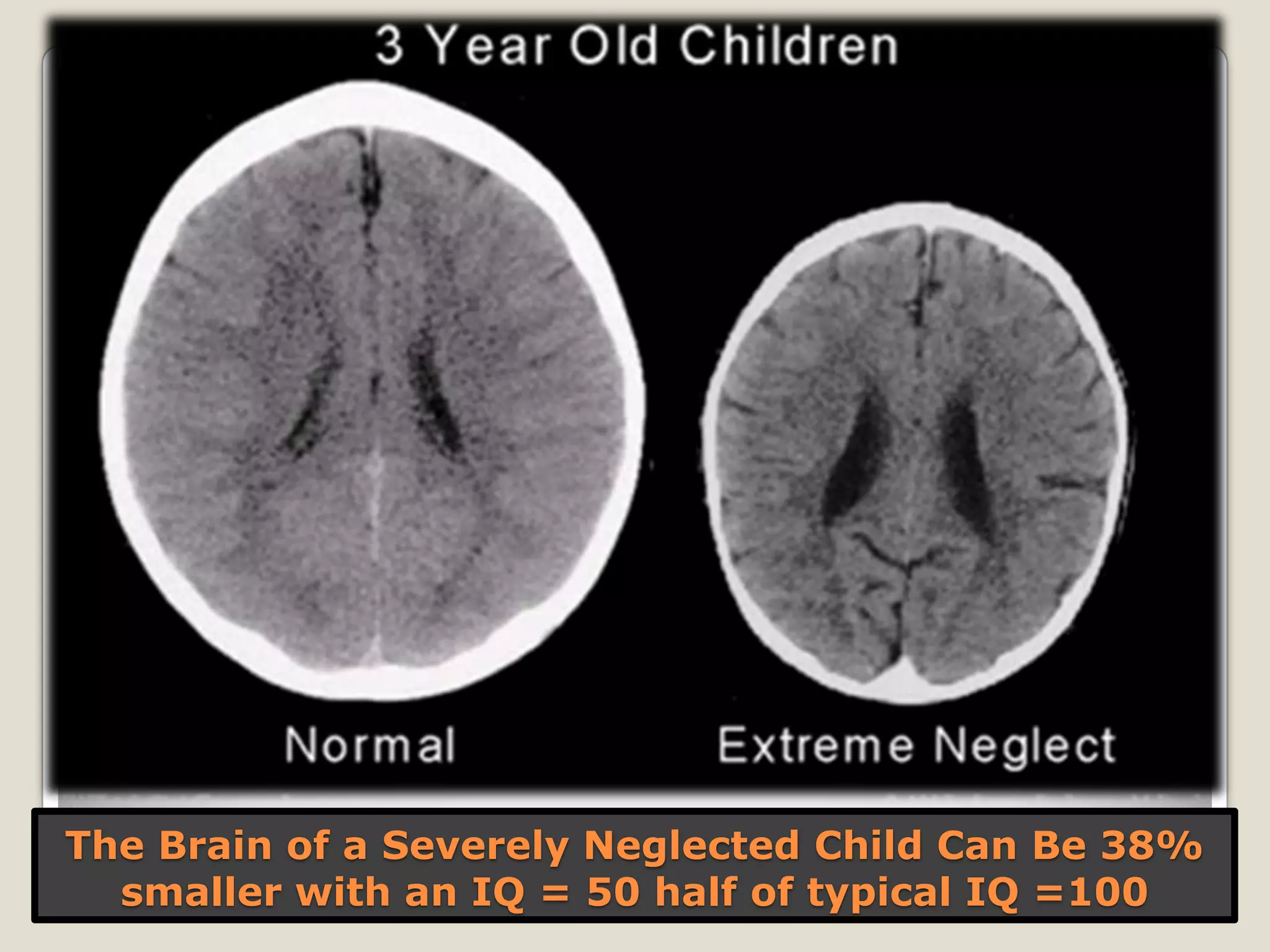
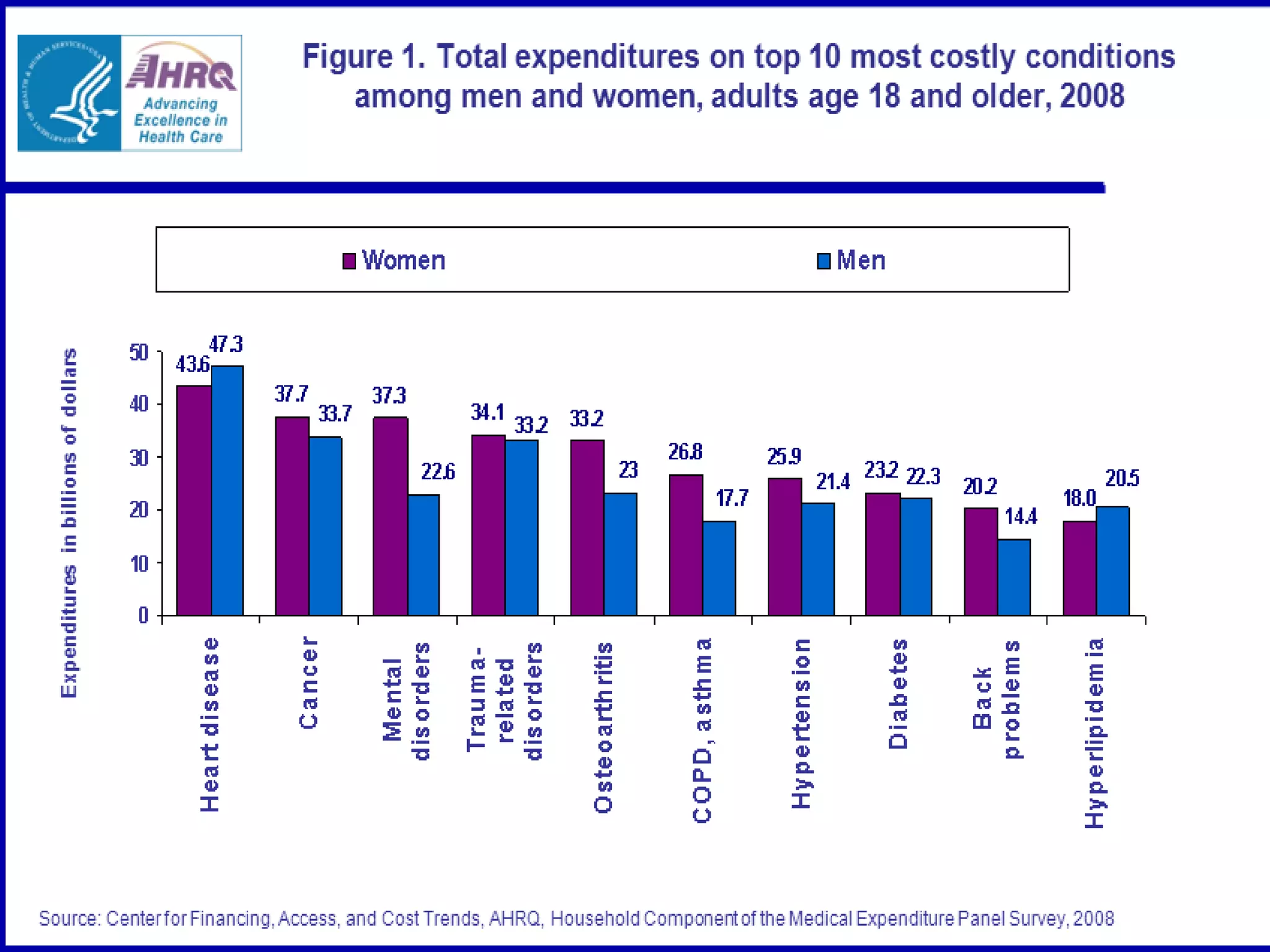
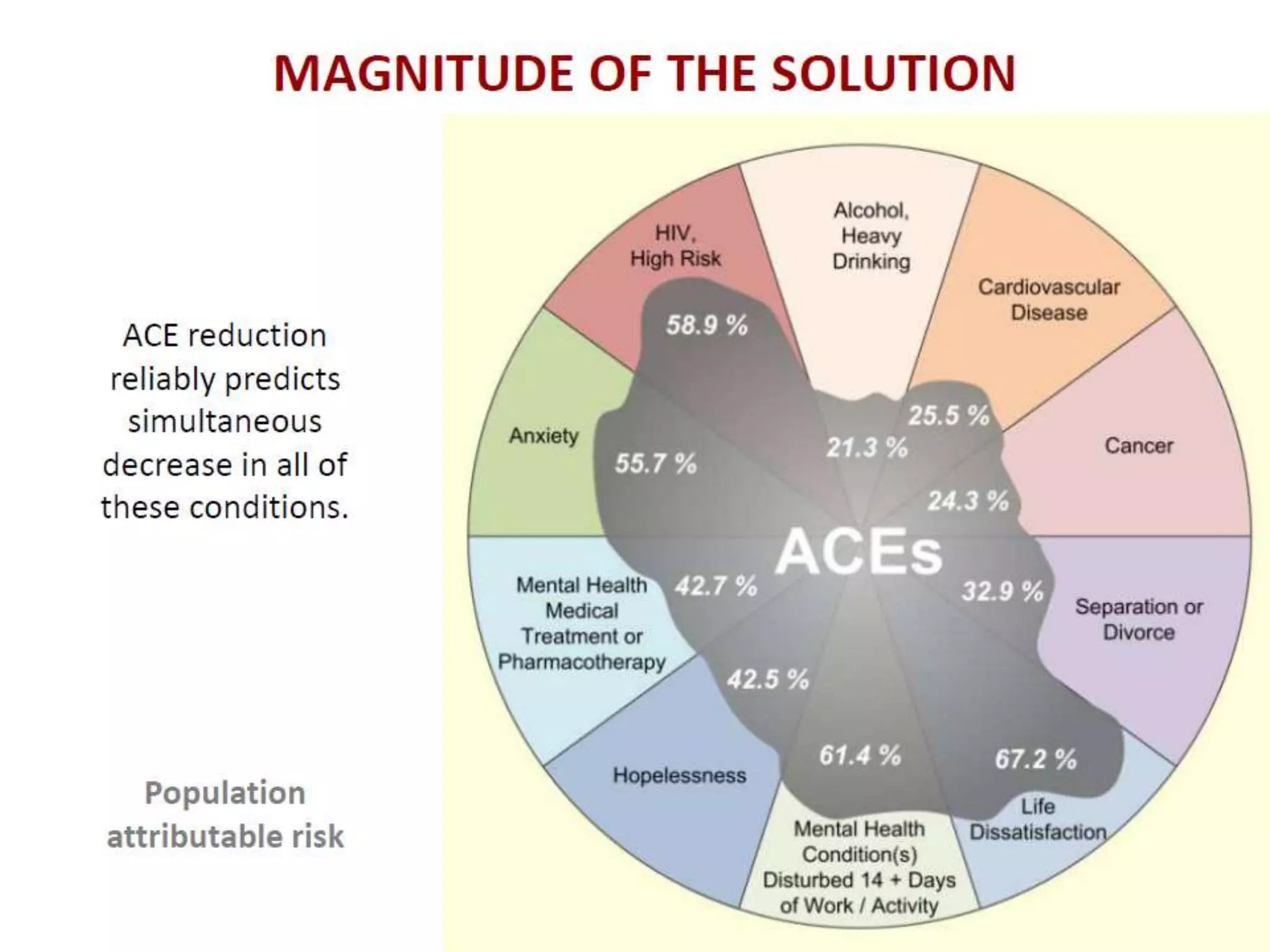
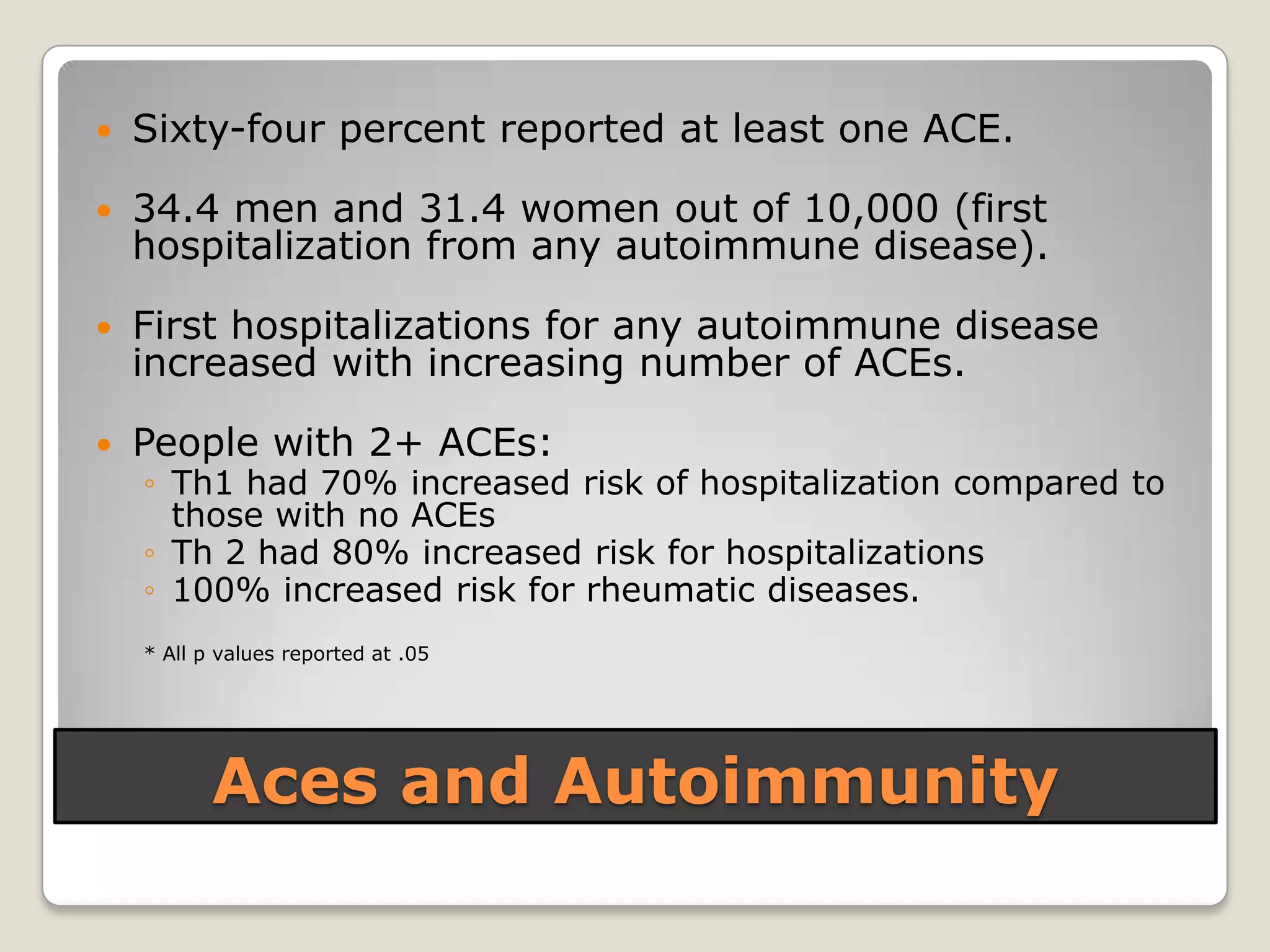
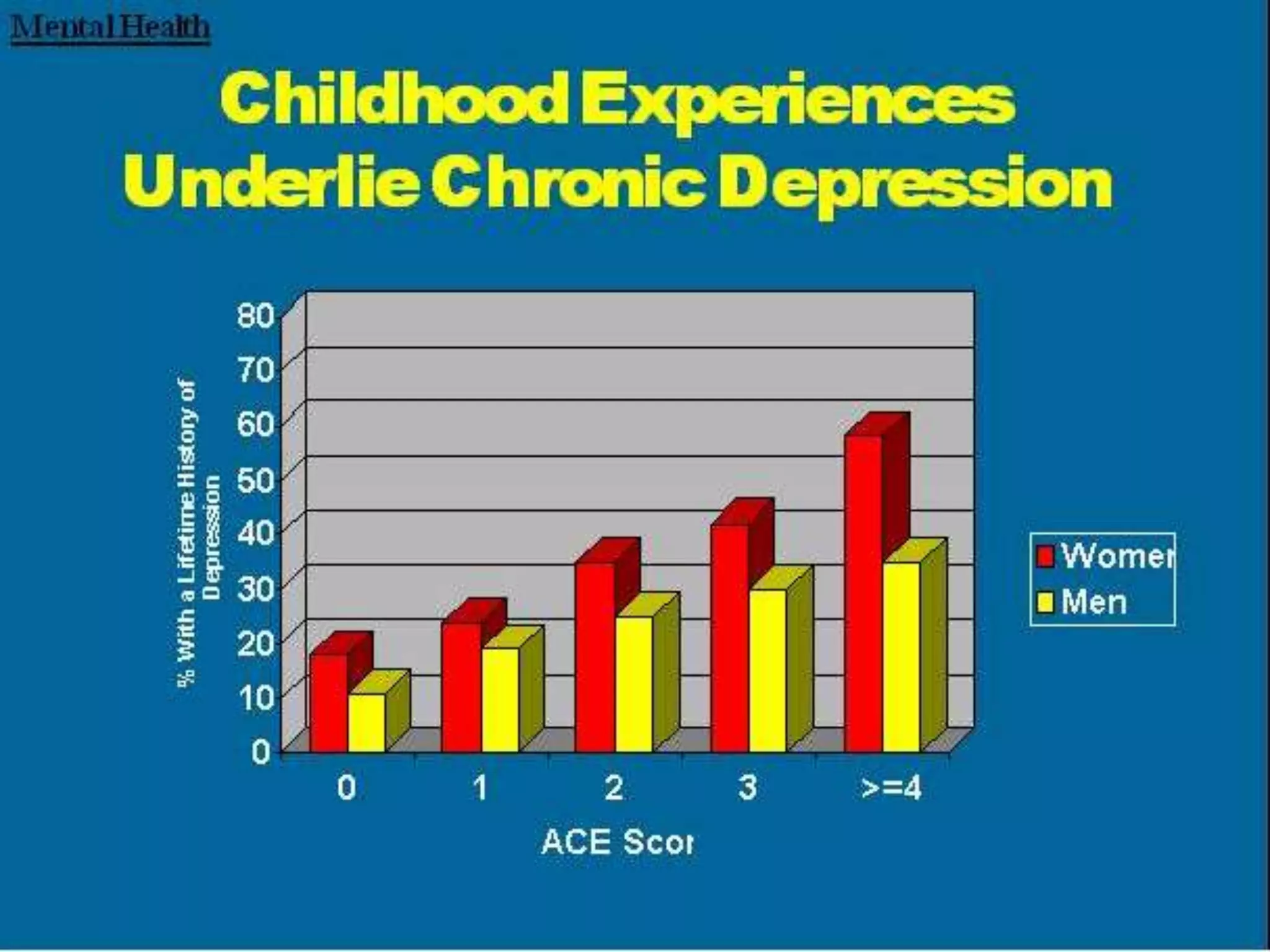
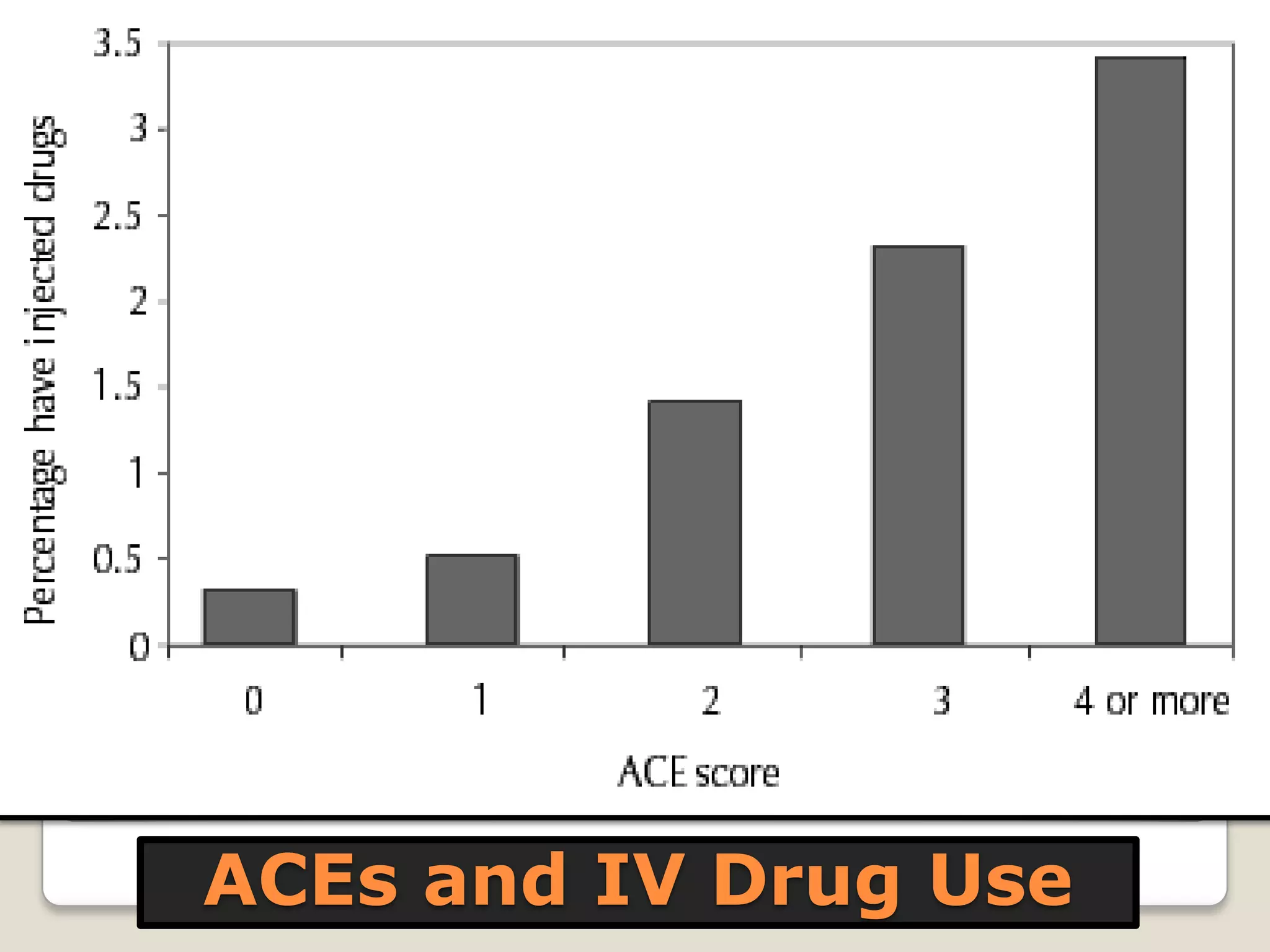
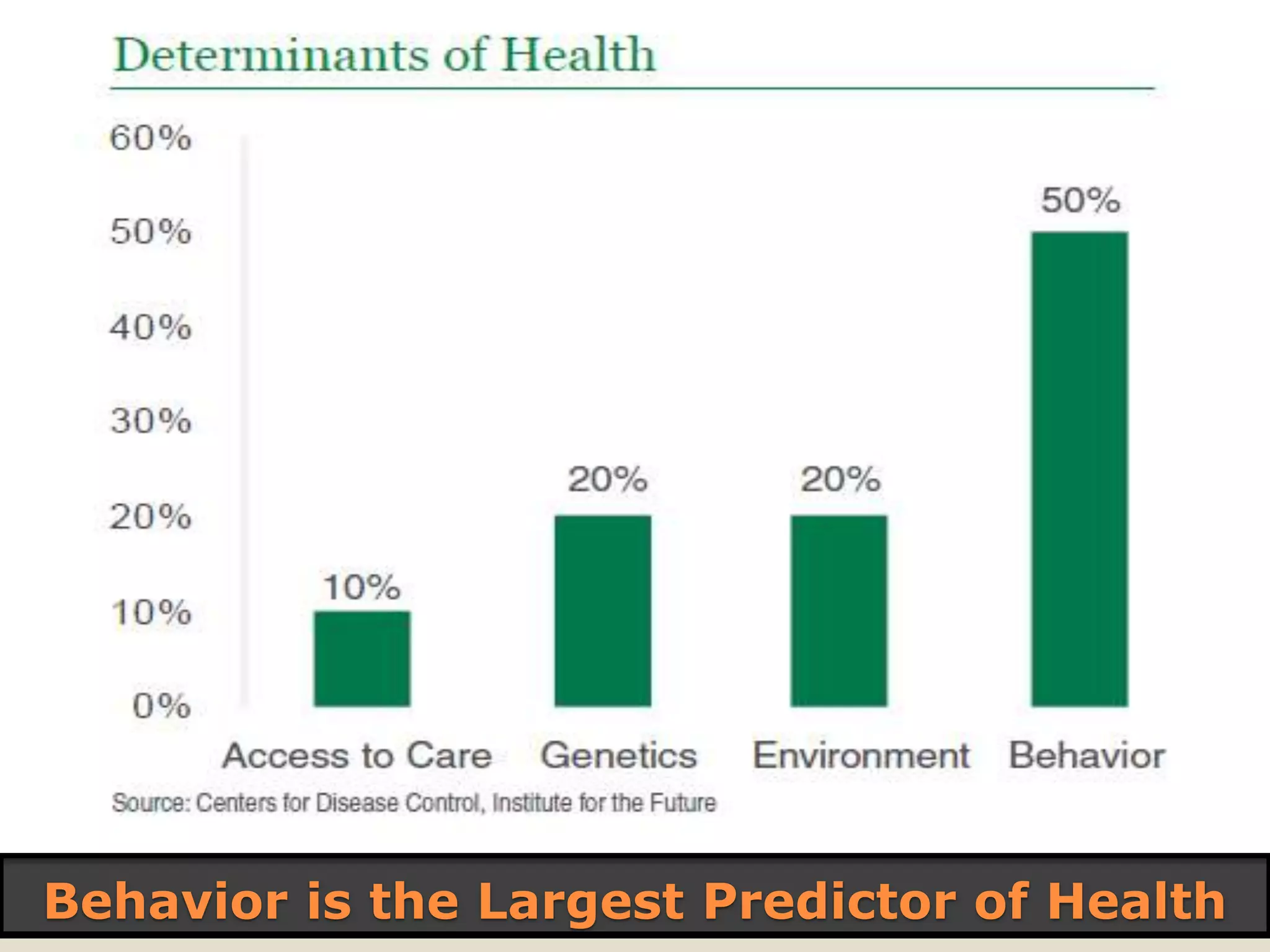
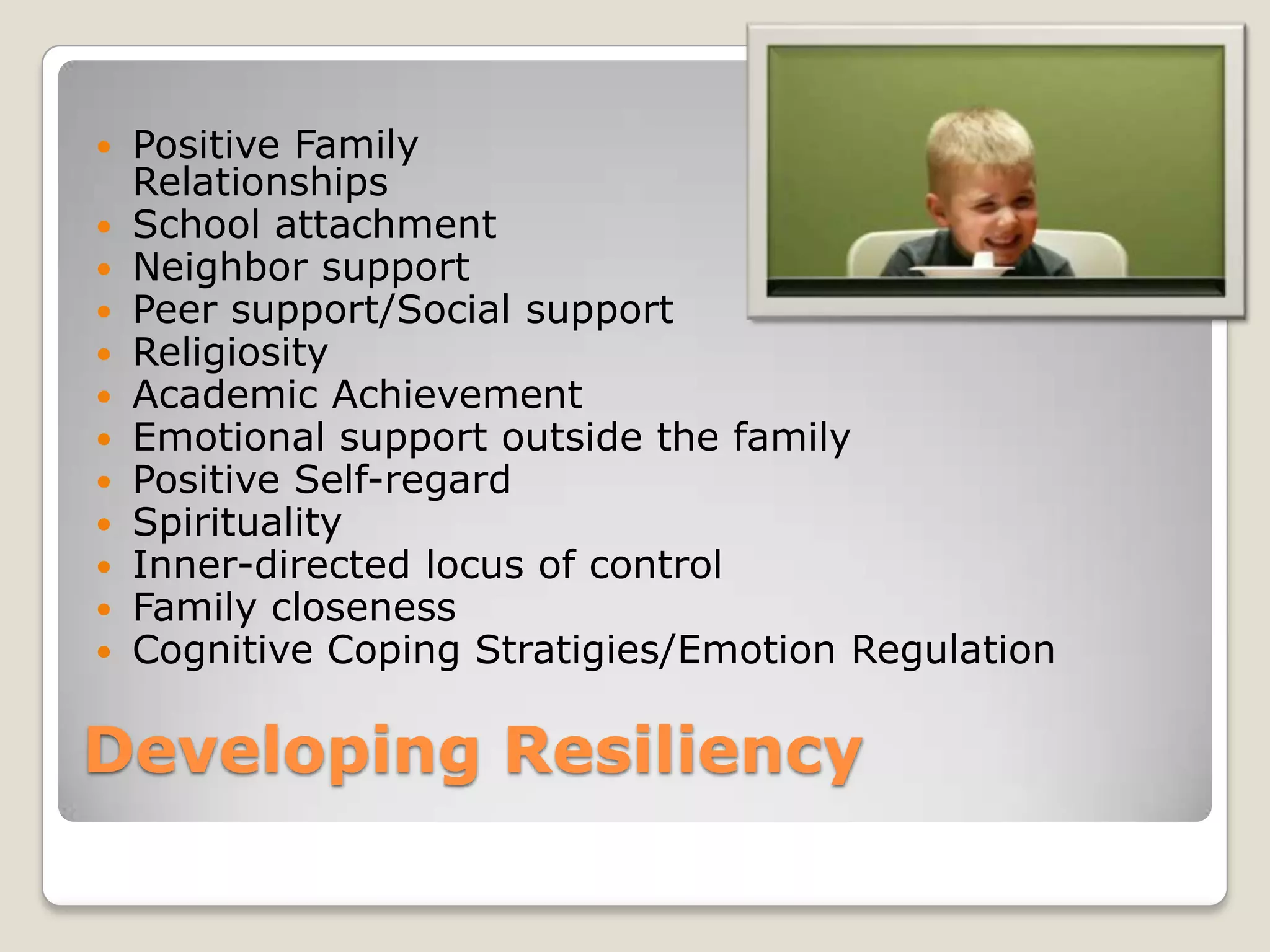
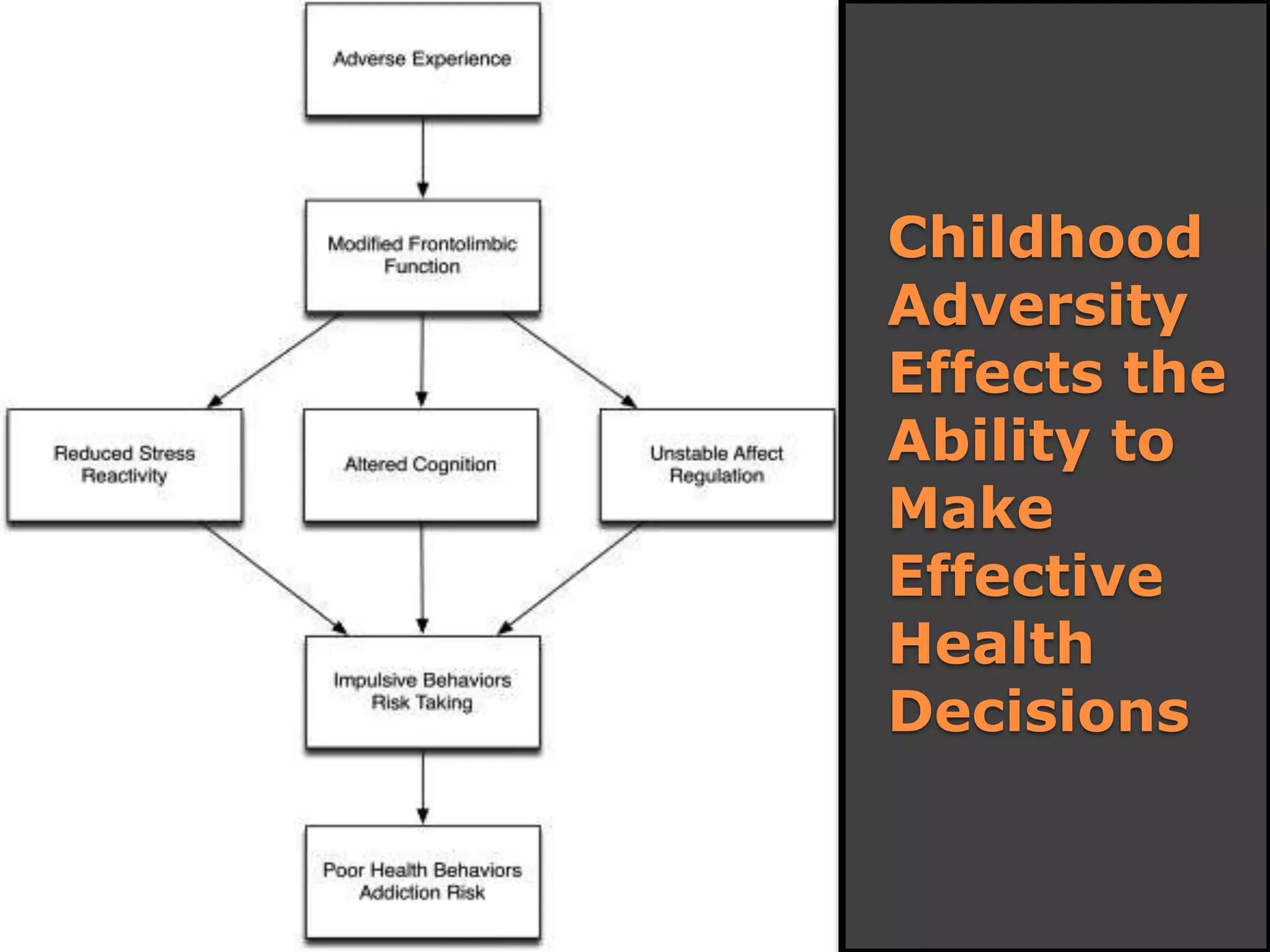
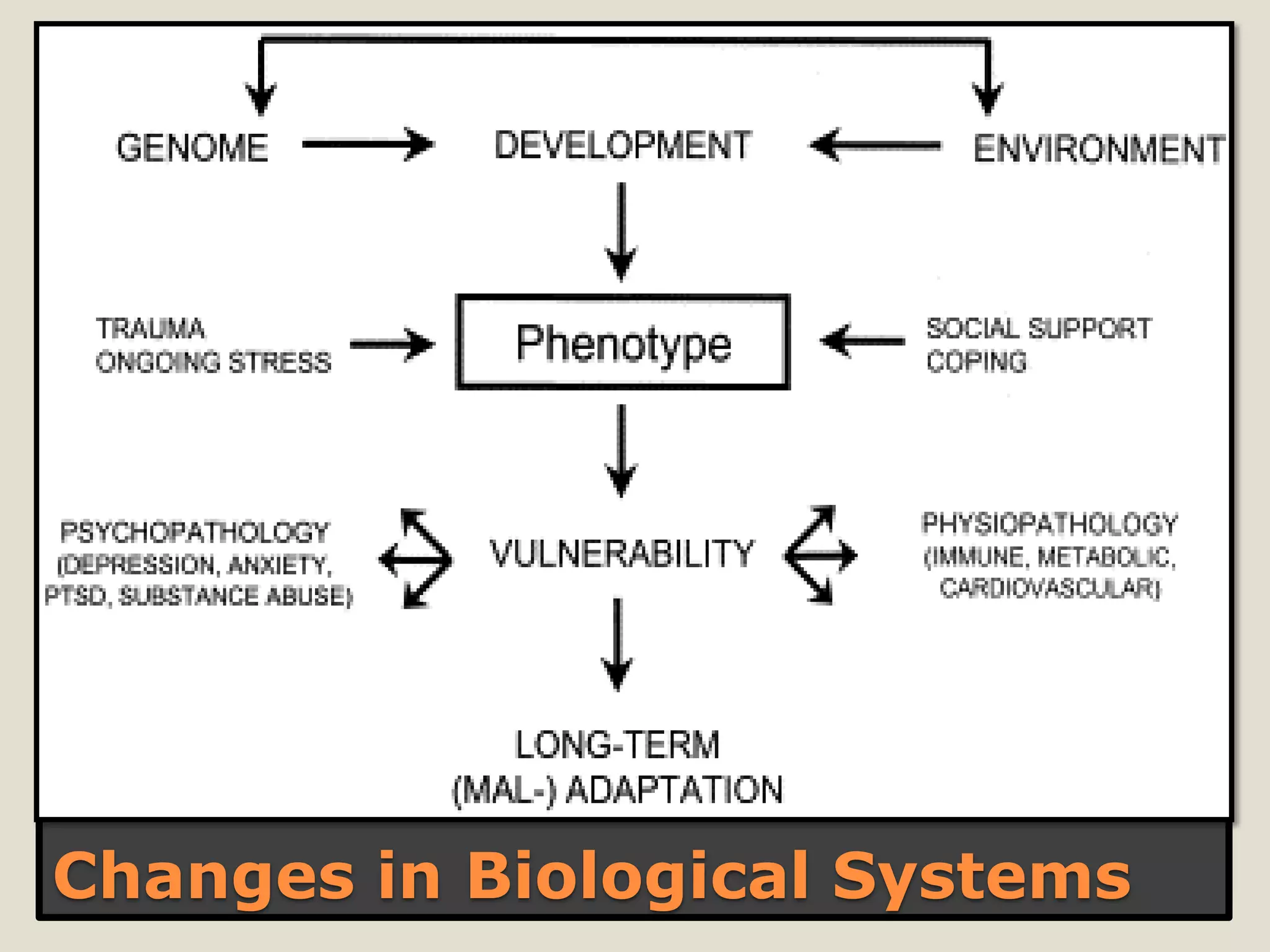
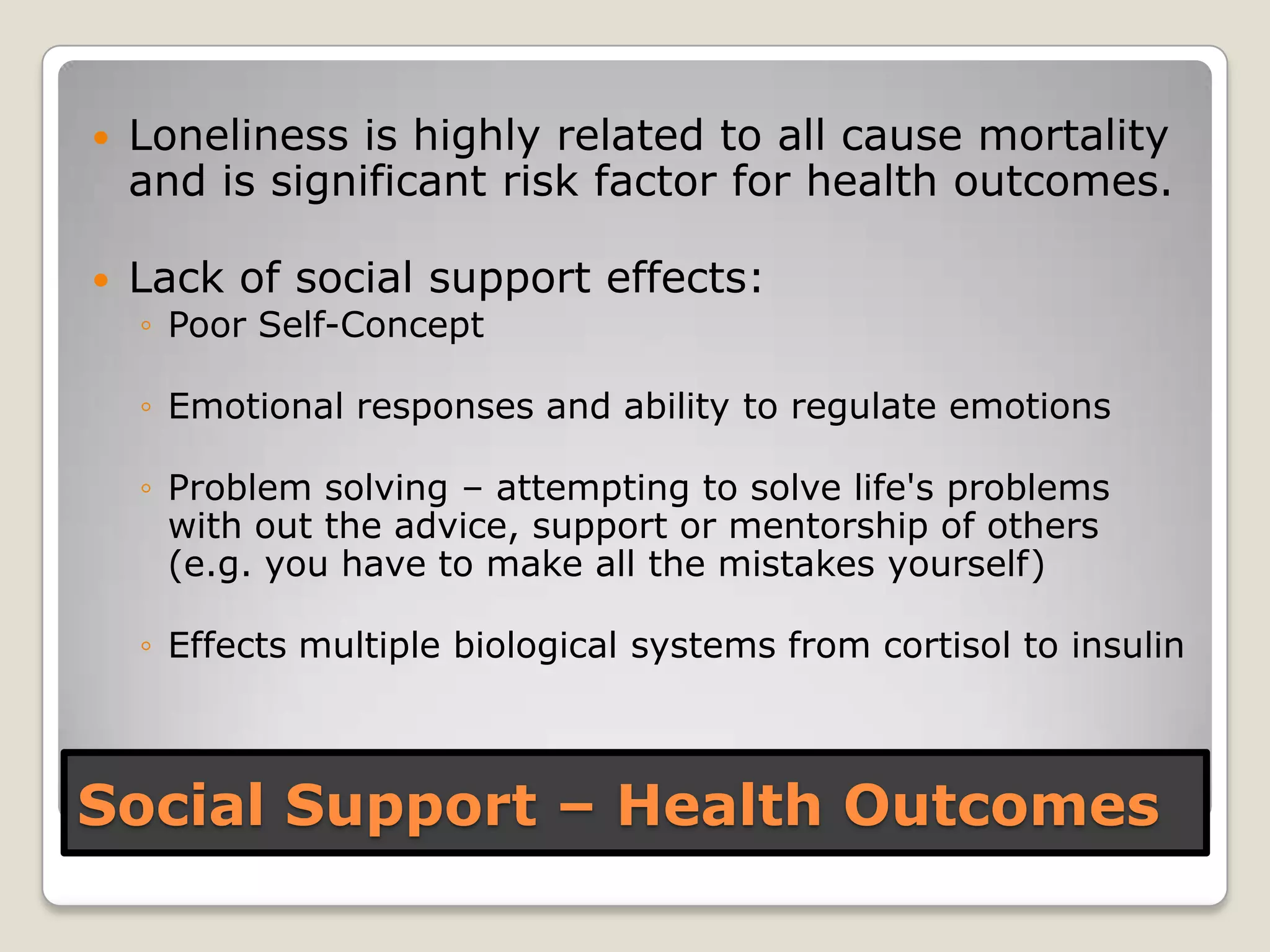
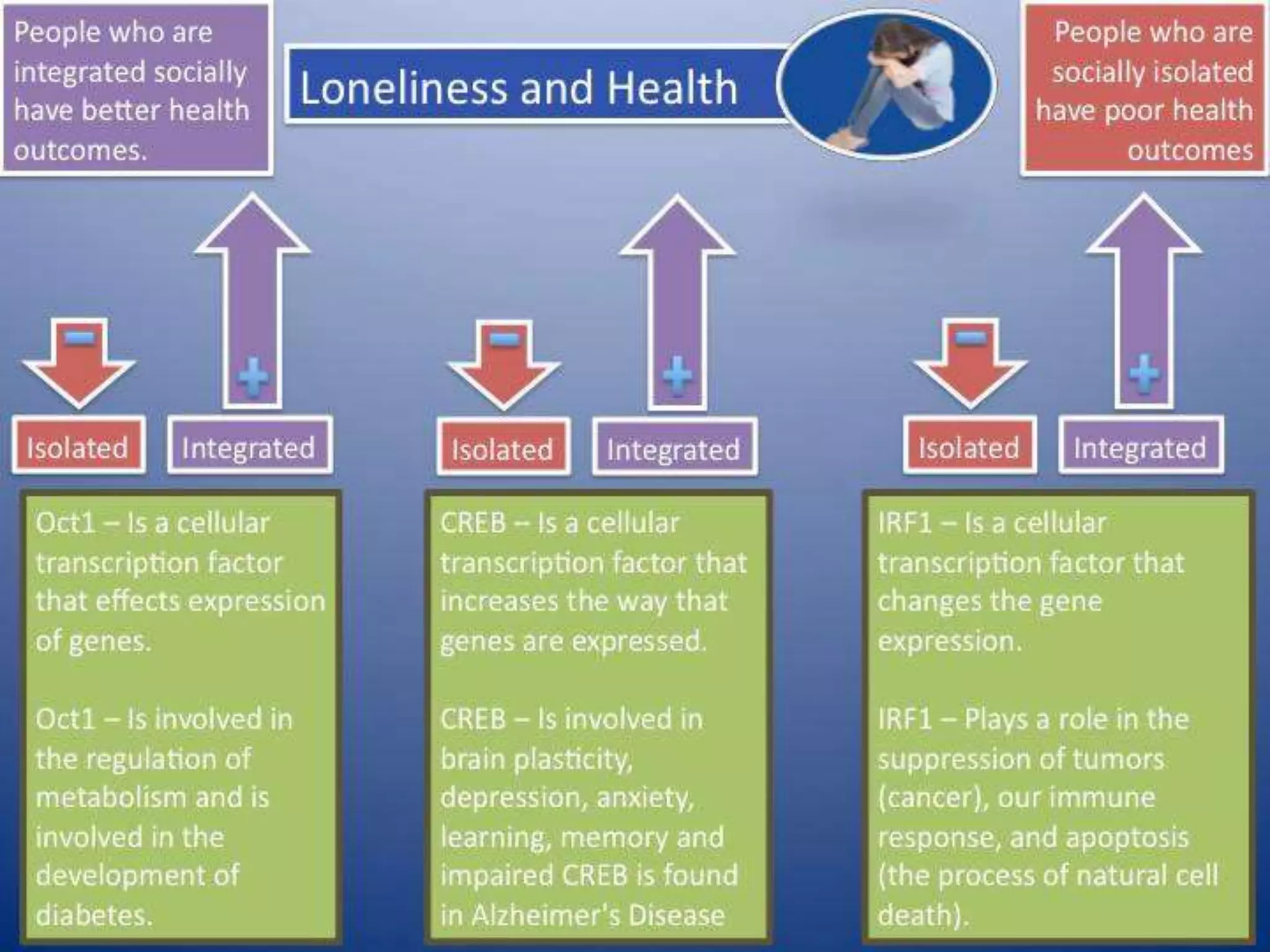
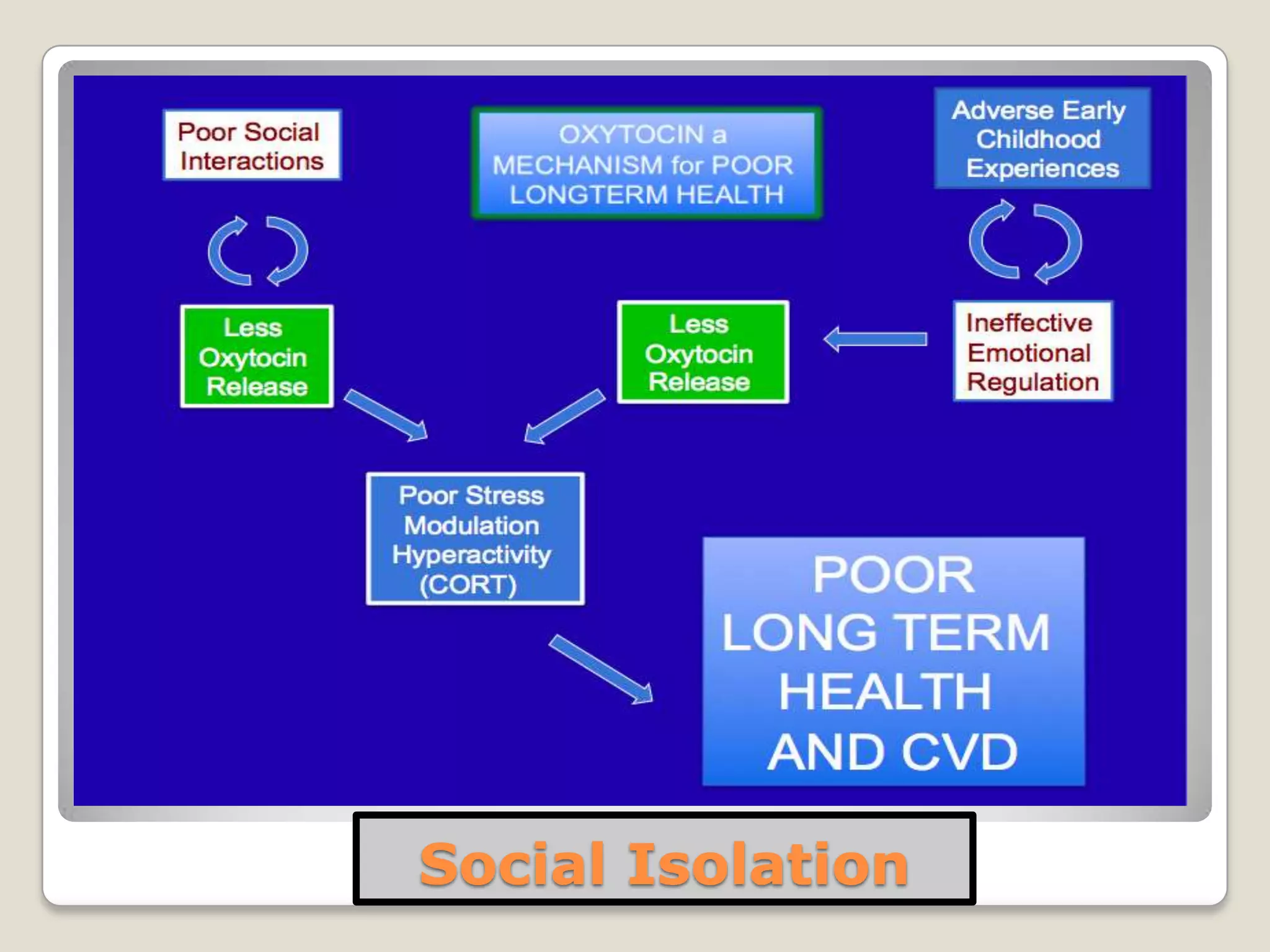
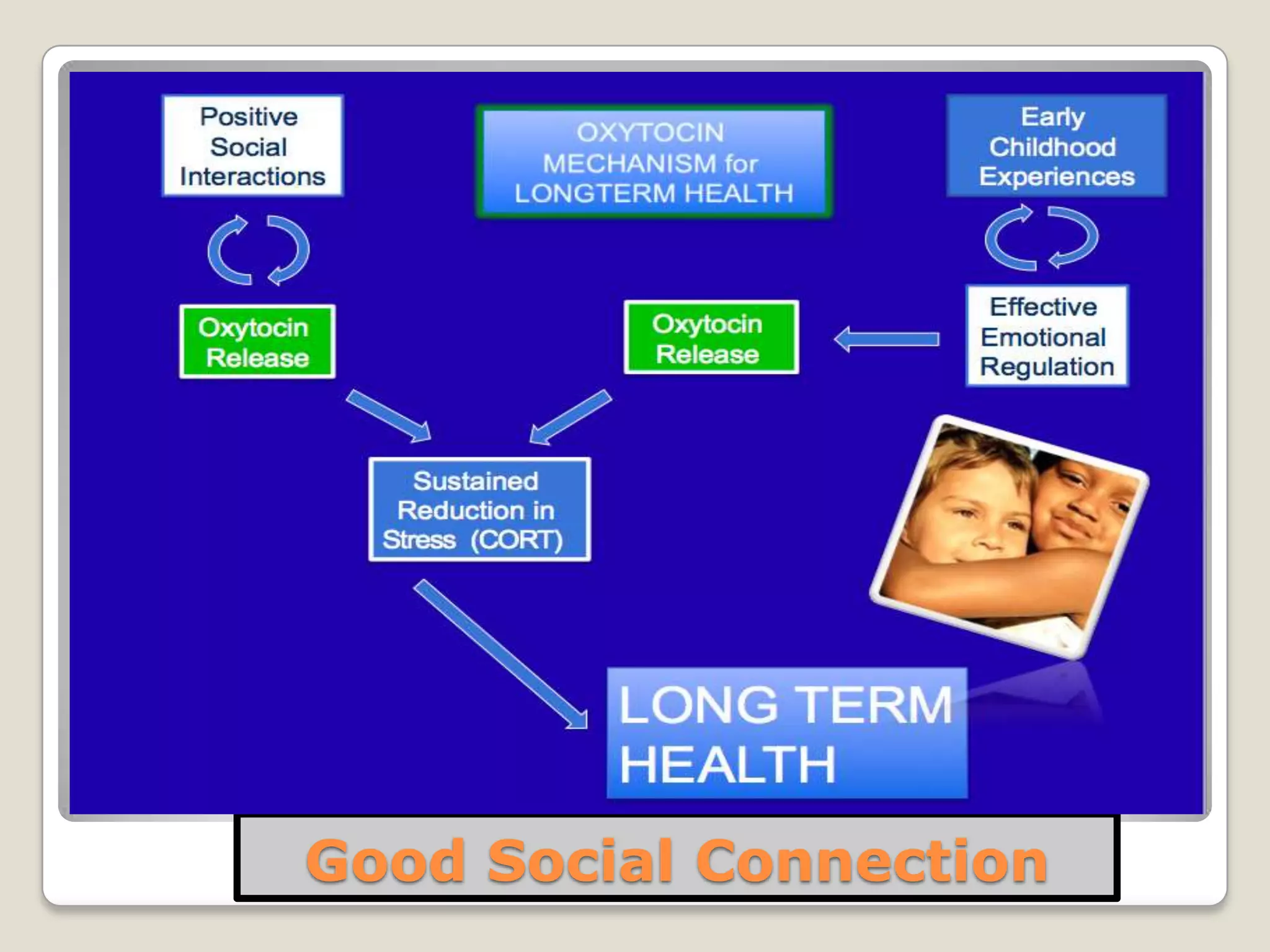
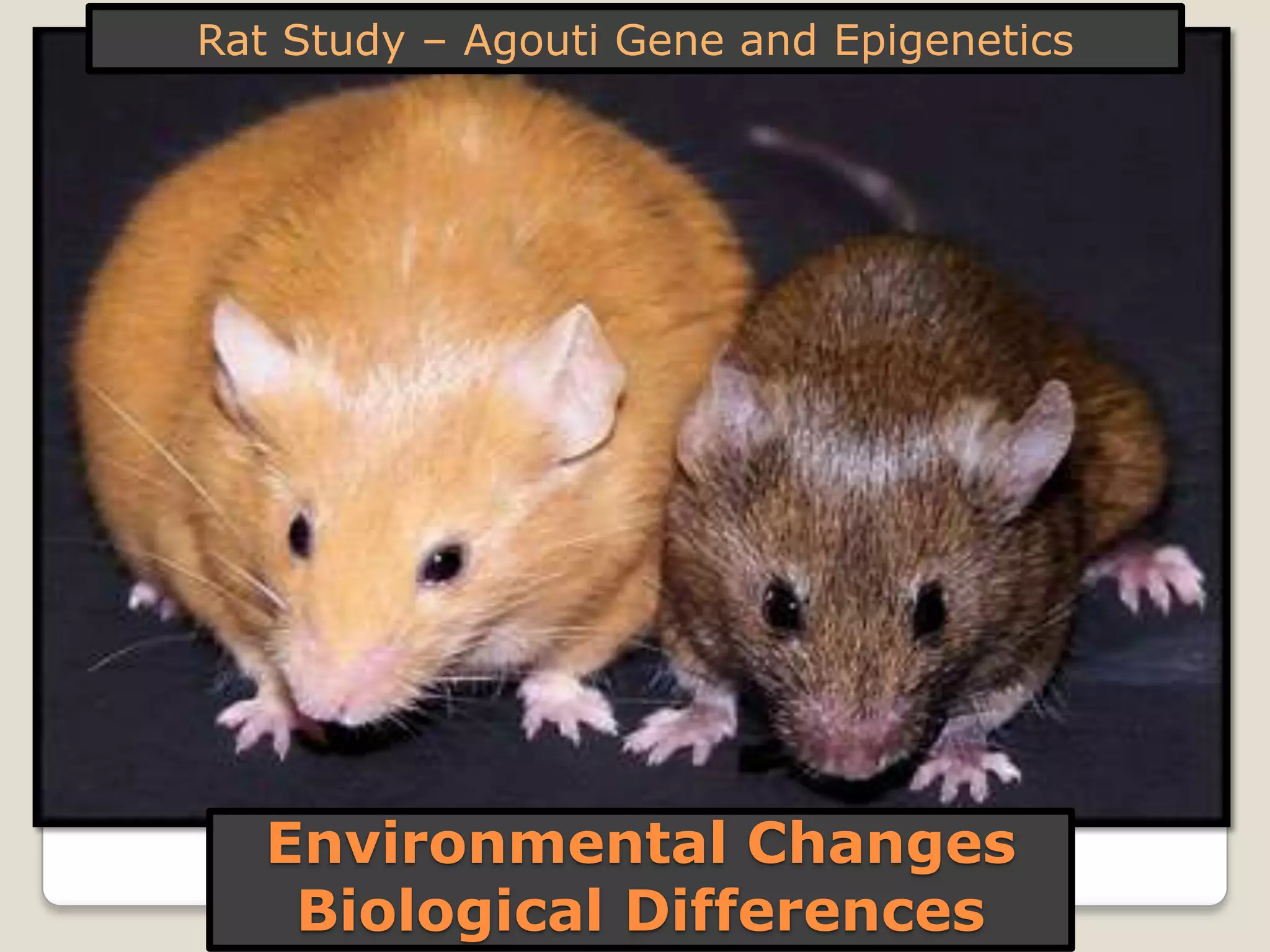
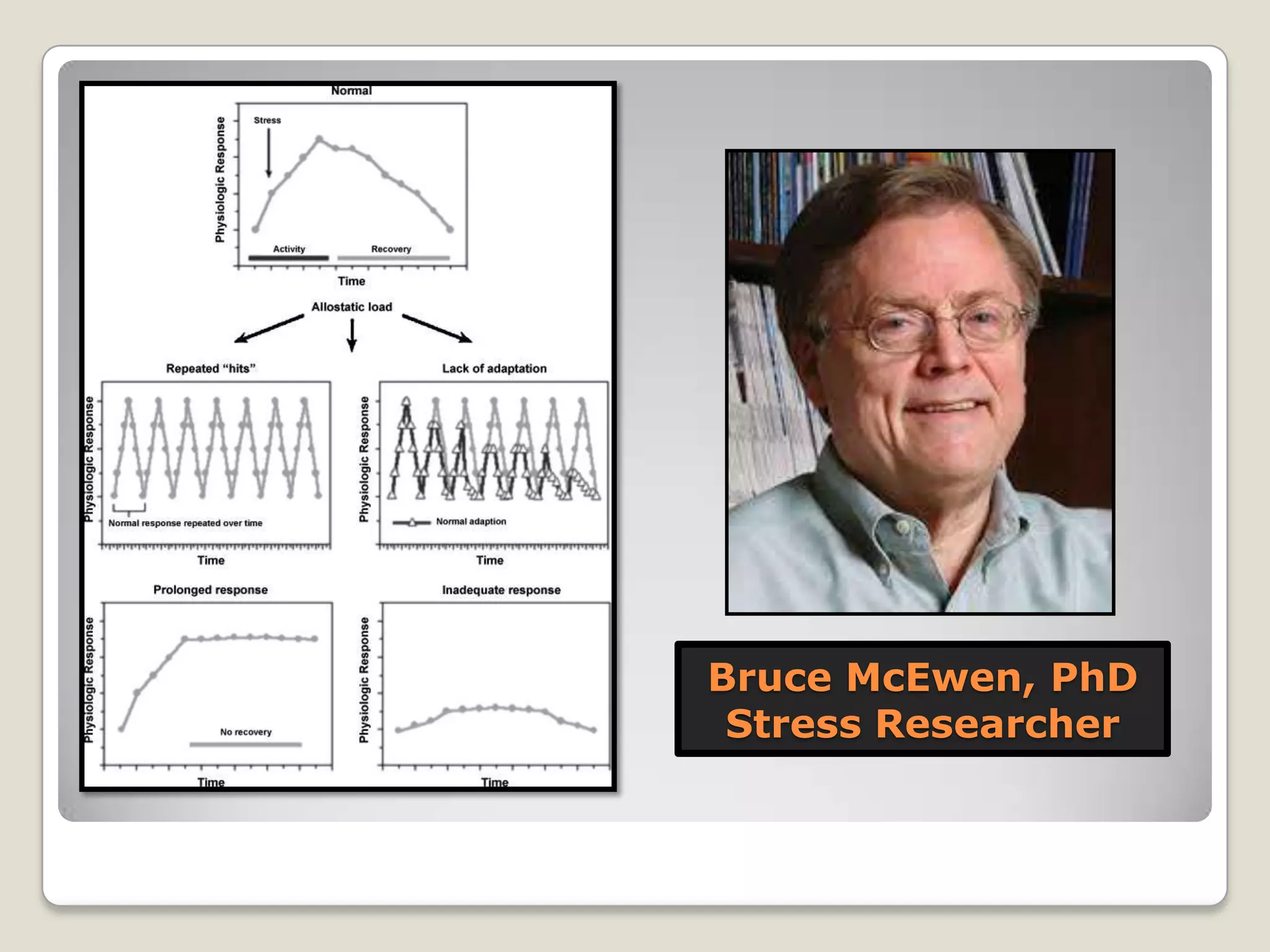
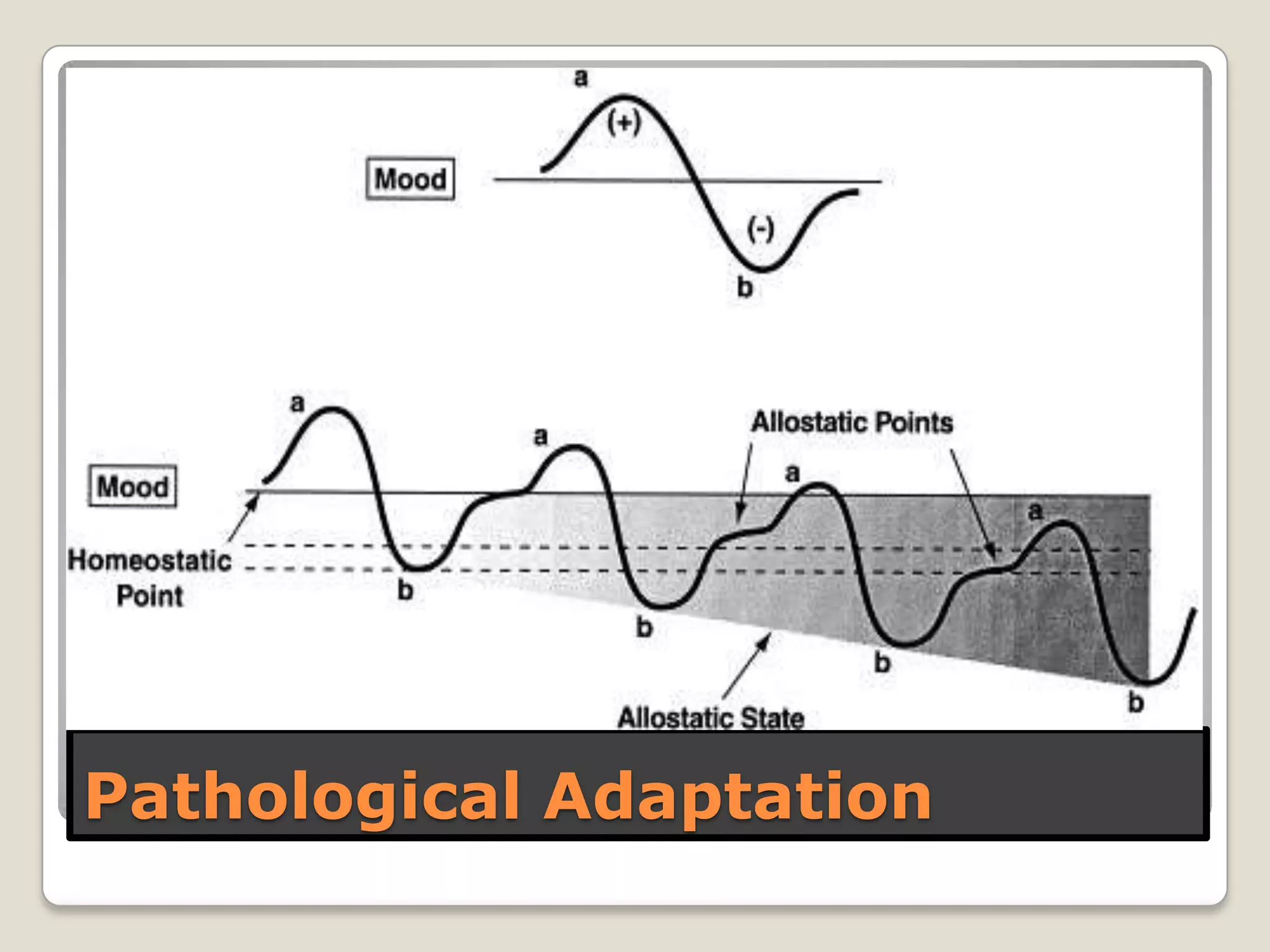
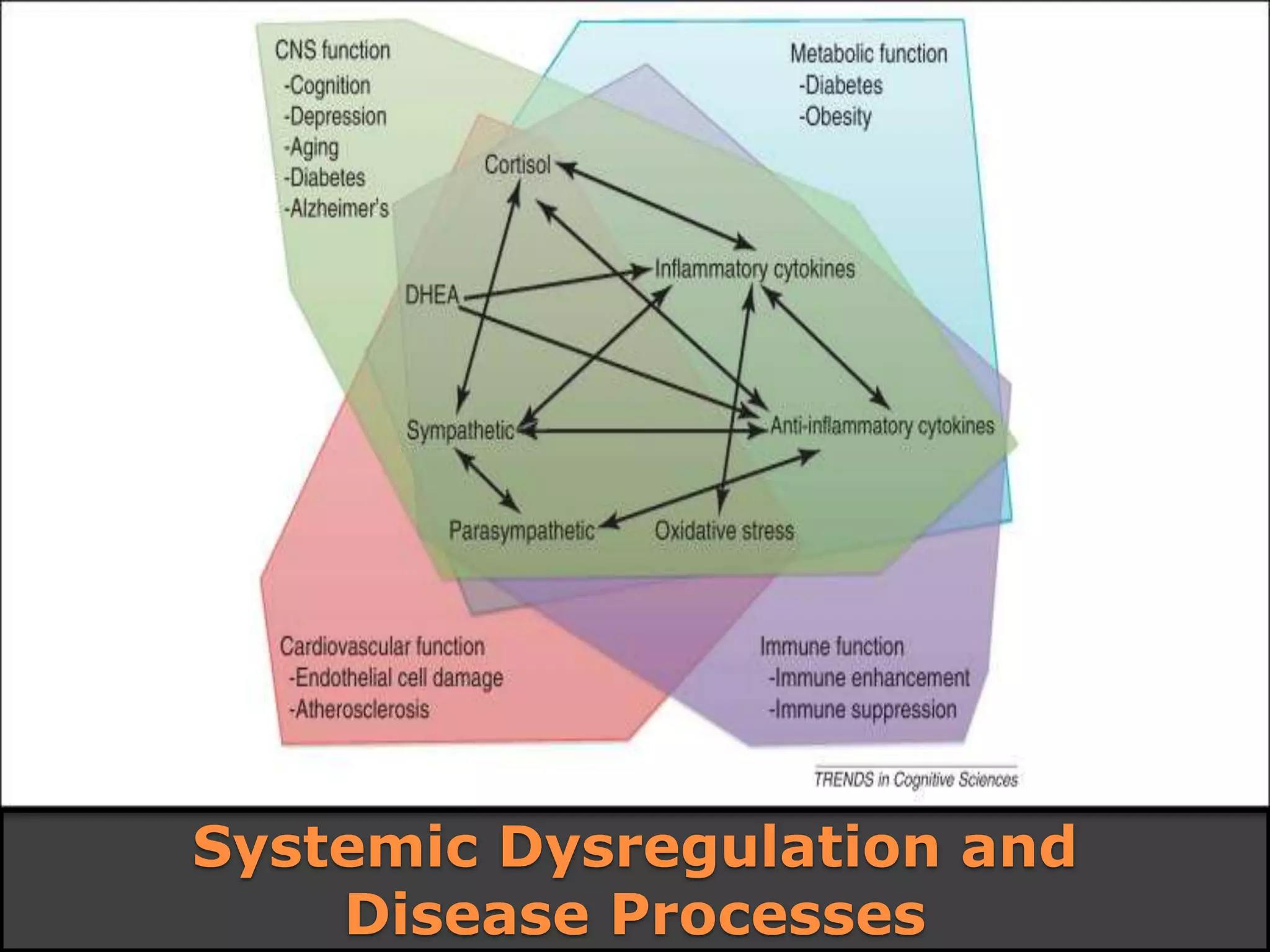
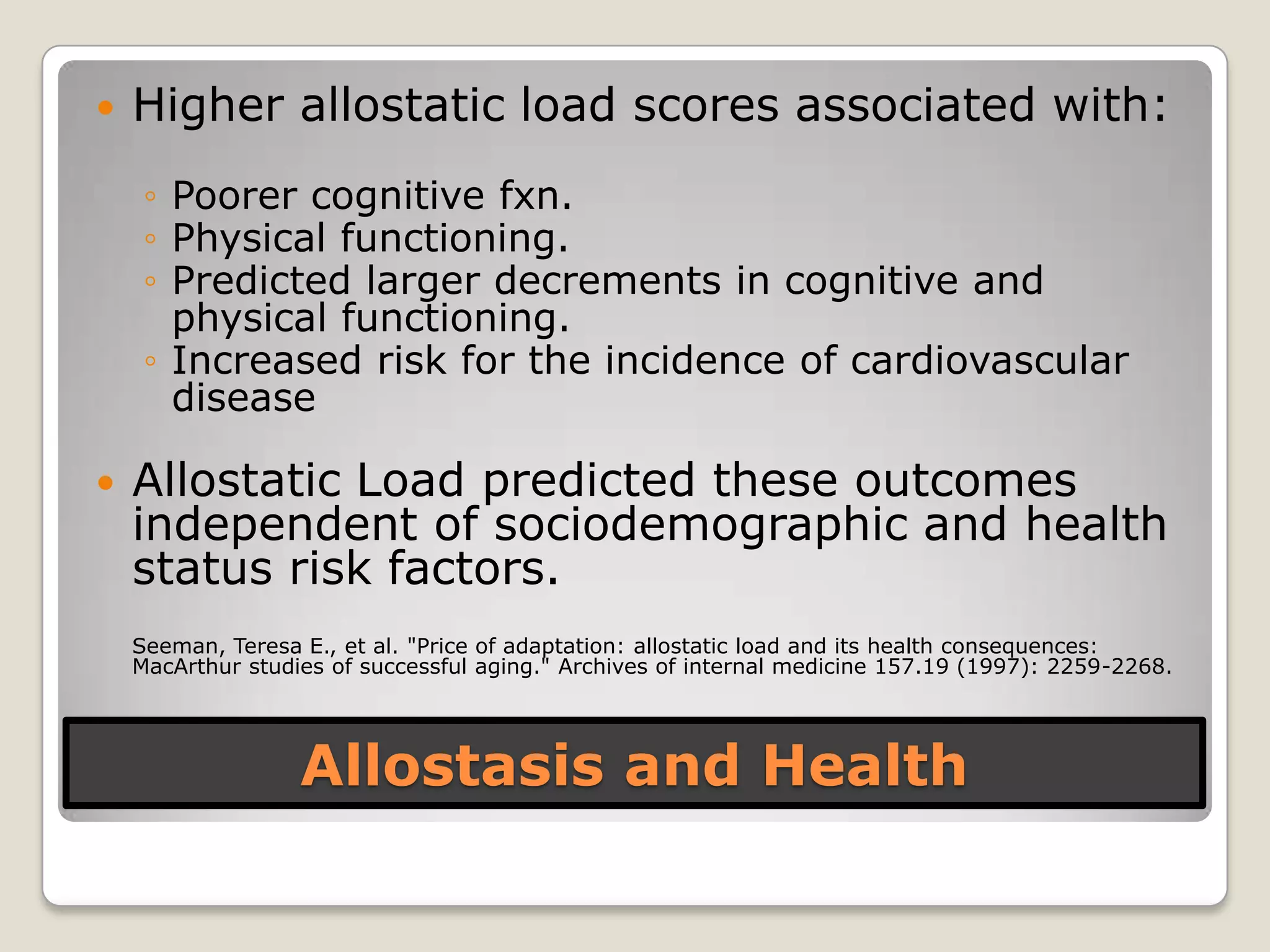
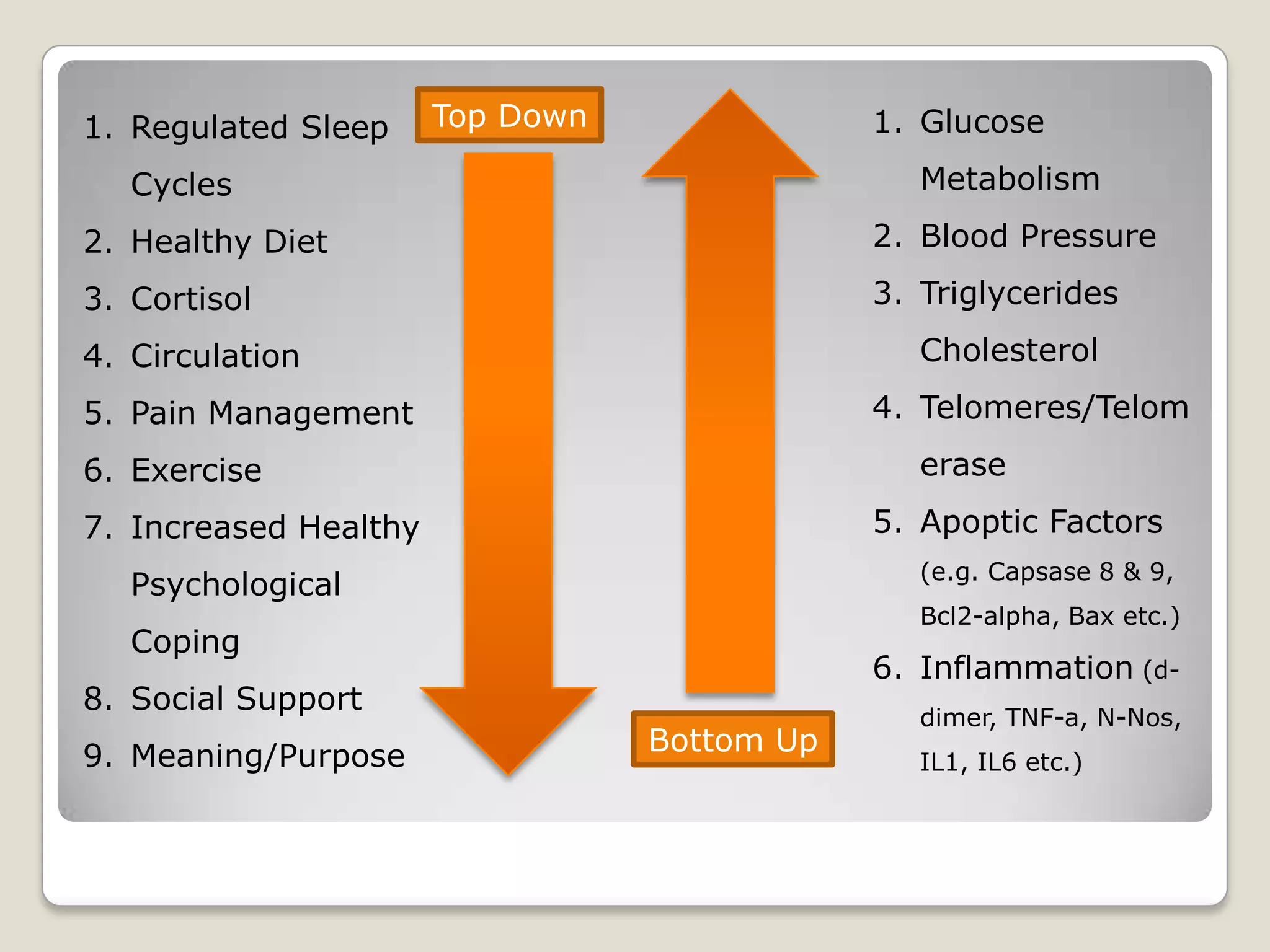
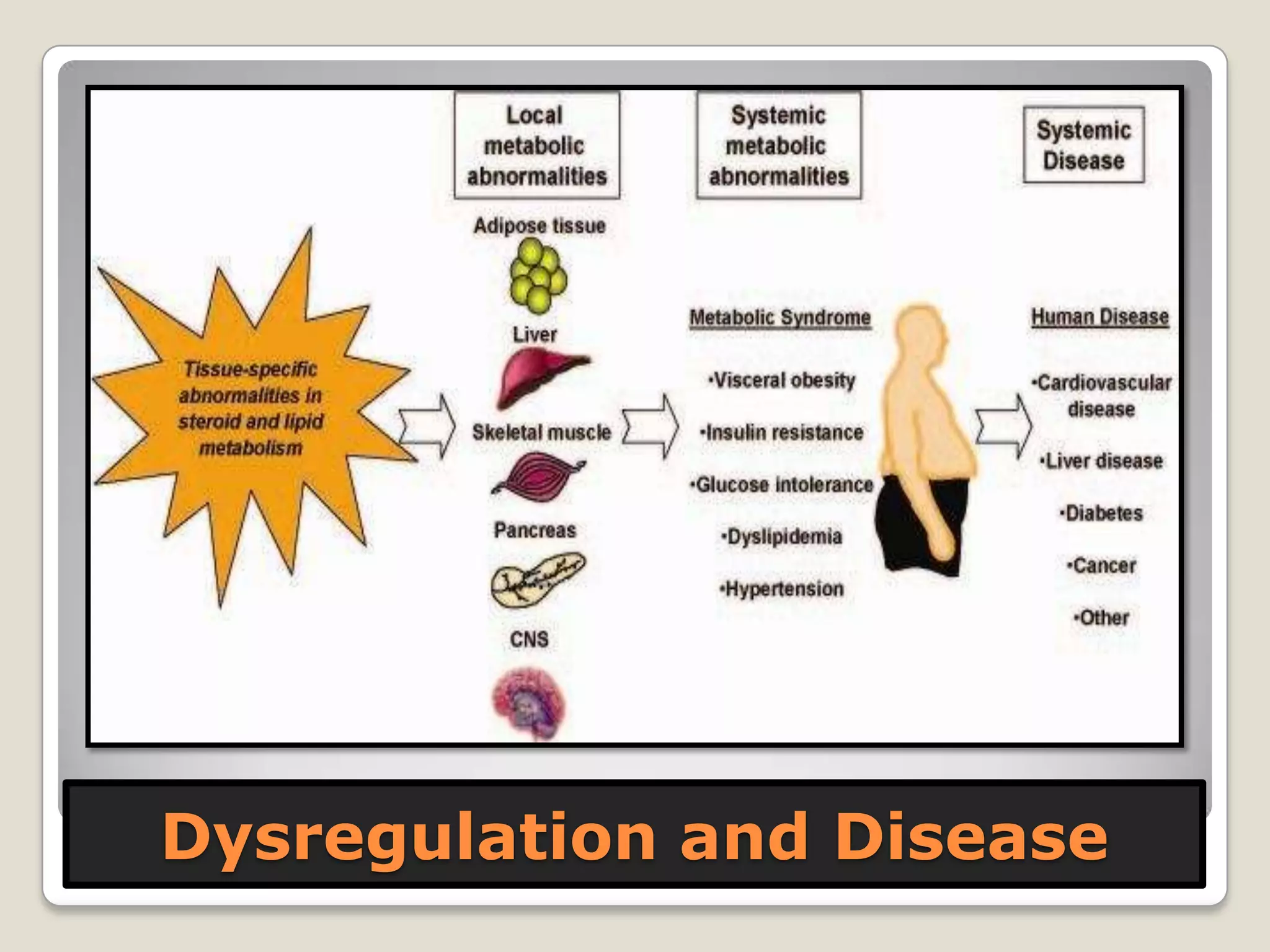
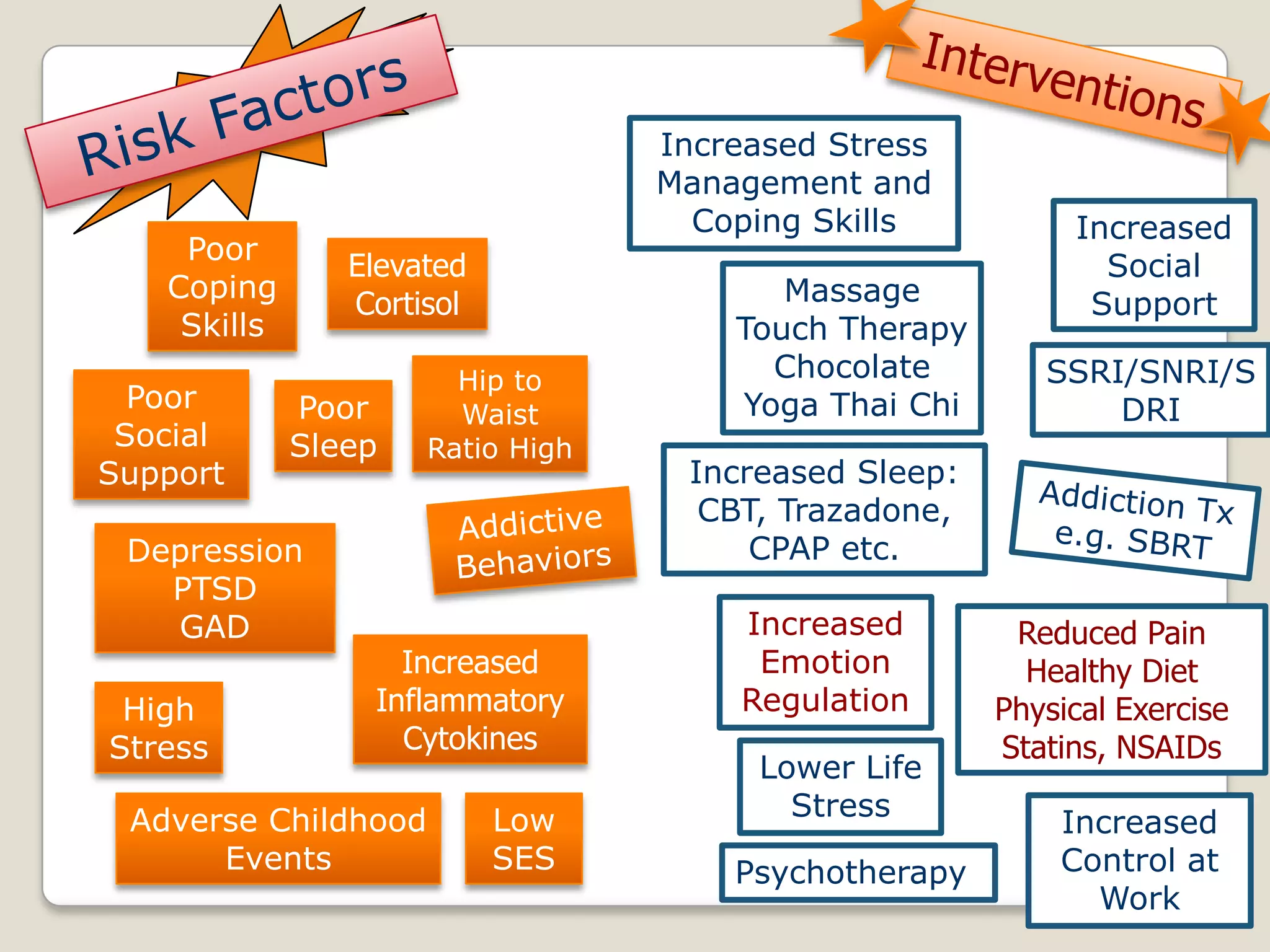
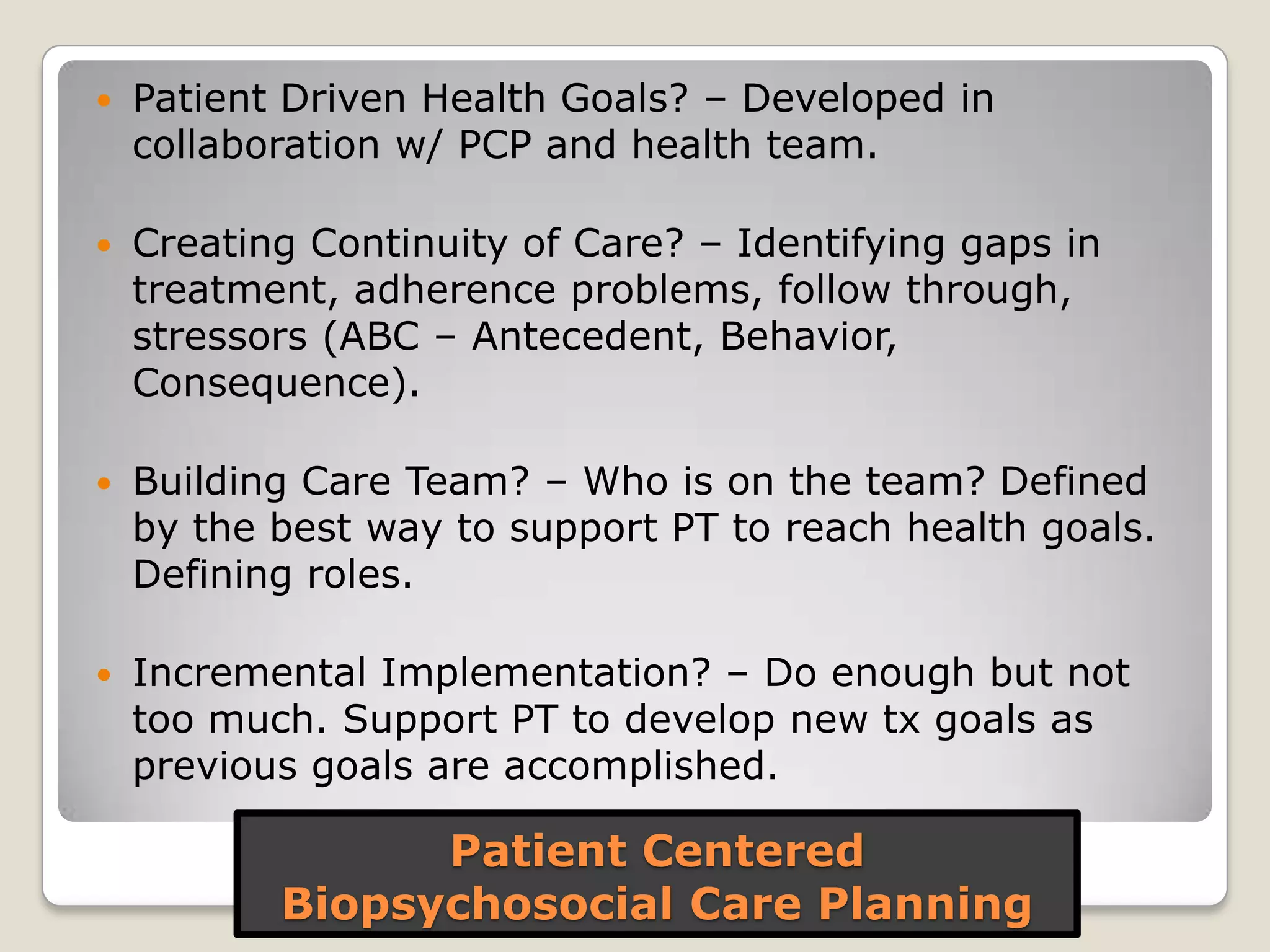
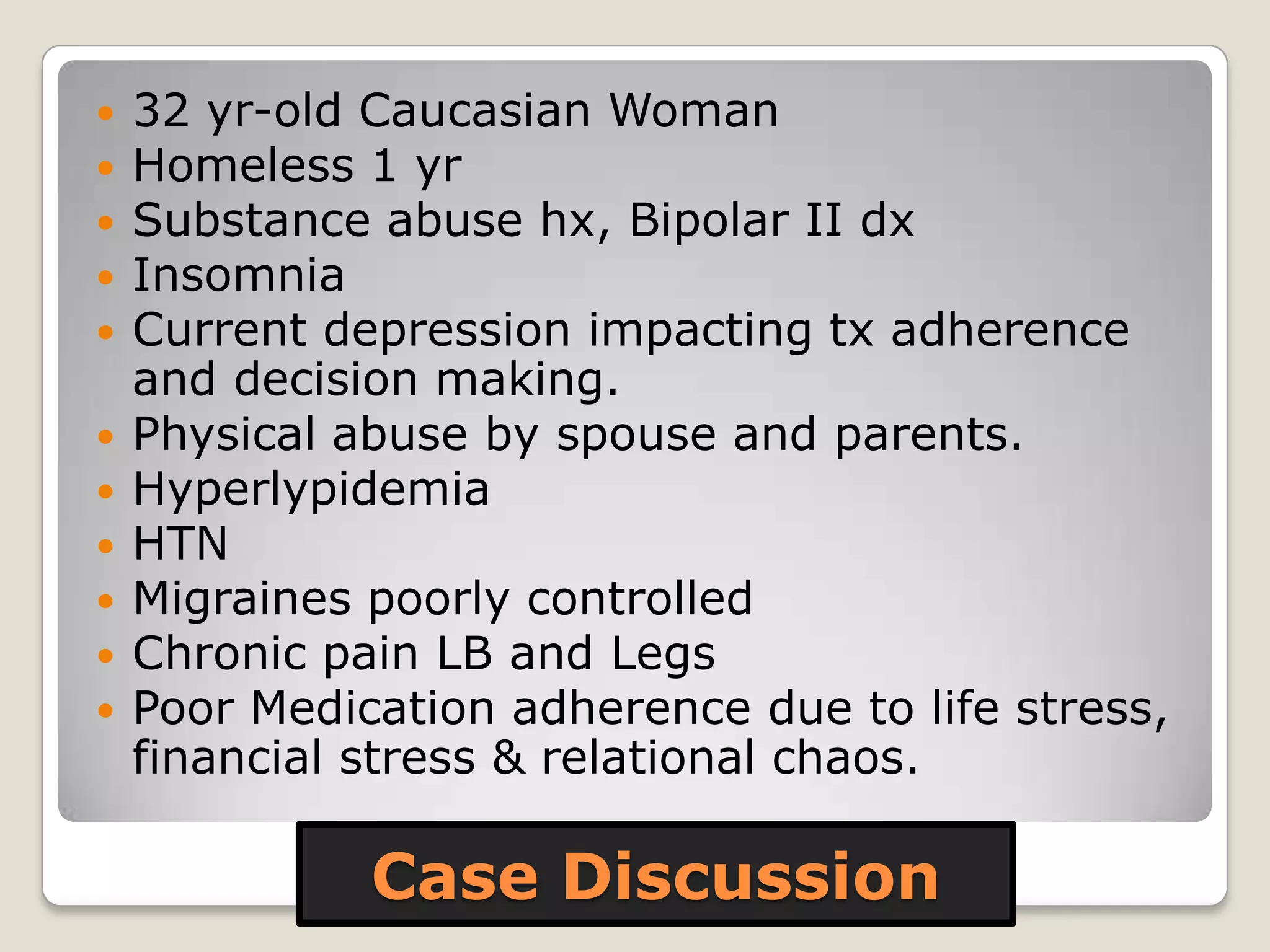
The document discusses childhood adversity and its impacts on health, emphasizing the biological and social pathways that lead to pathology. It highlights significant statistics regarding the effects of adversity, such as increased risks of autoimmune diseases and depression, and proposes clinical tools to address these consequences. Key factors for resilience include strong social support, positive family relationships, and effective coping strategies.