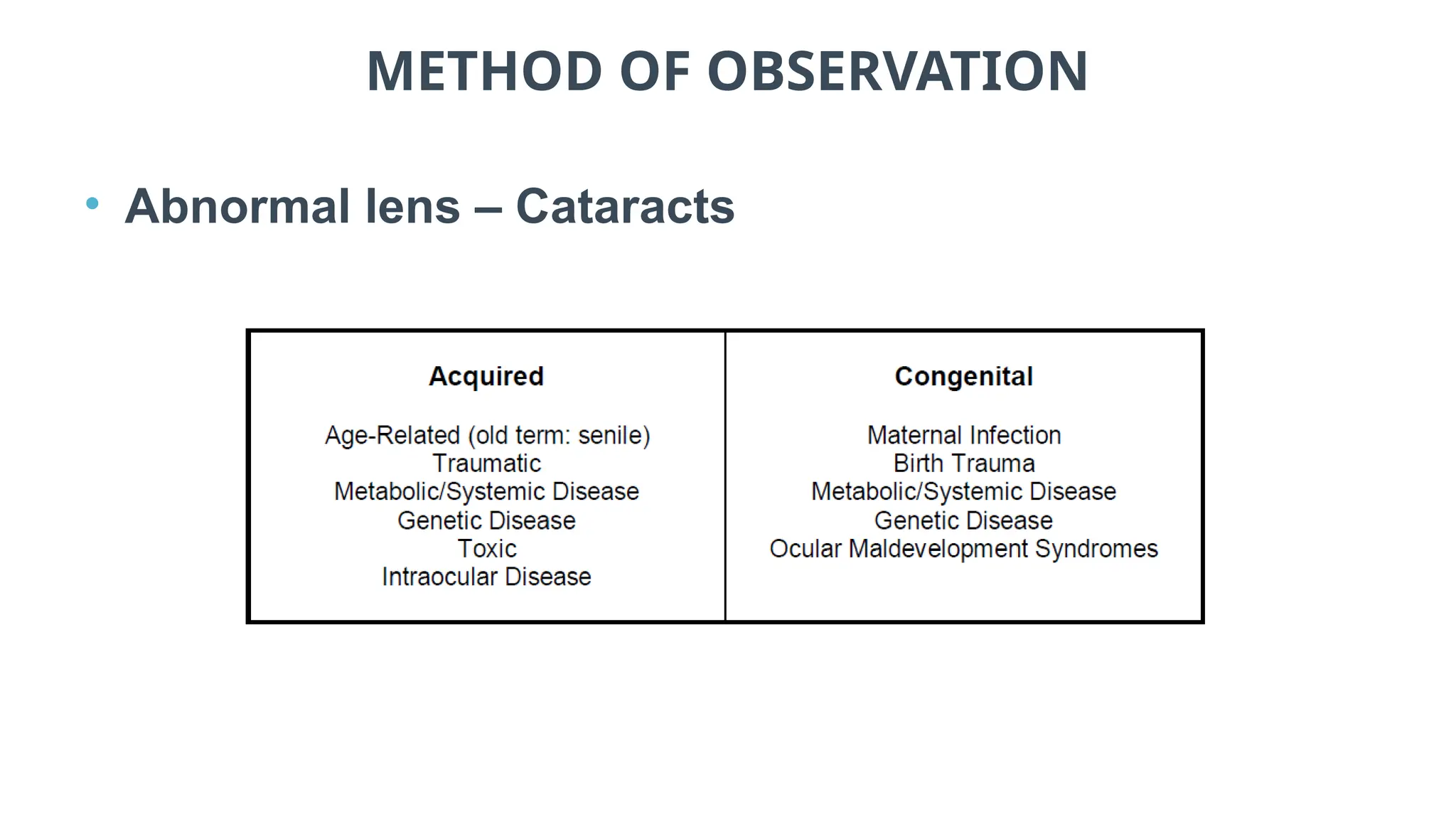
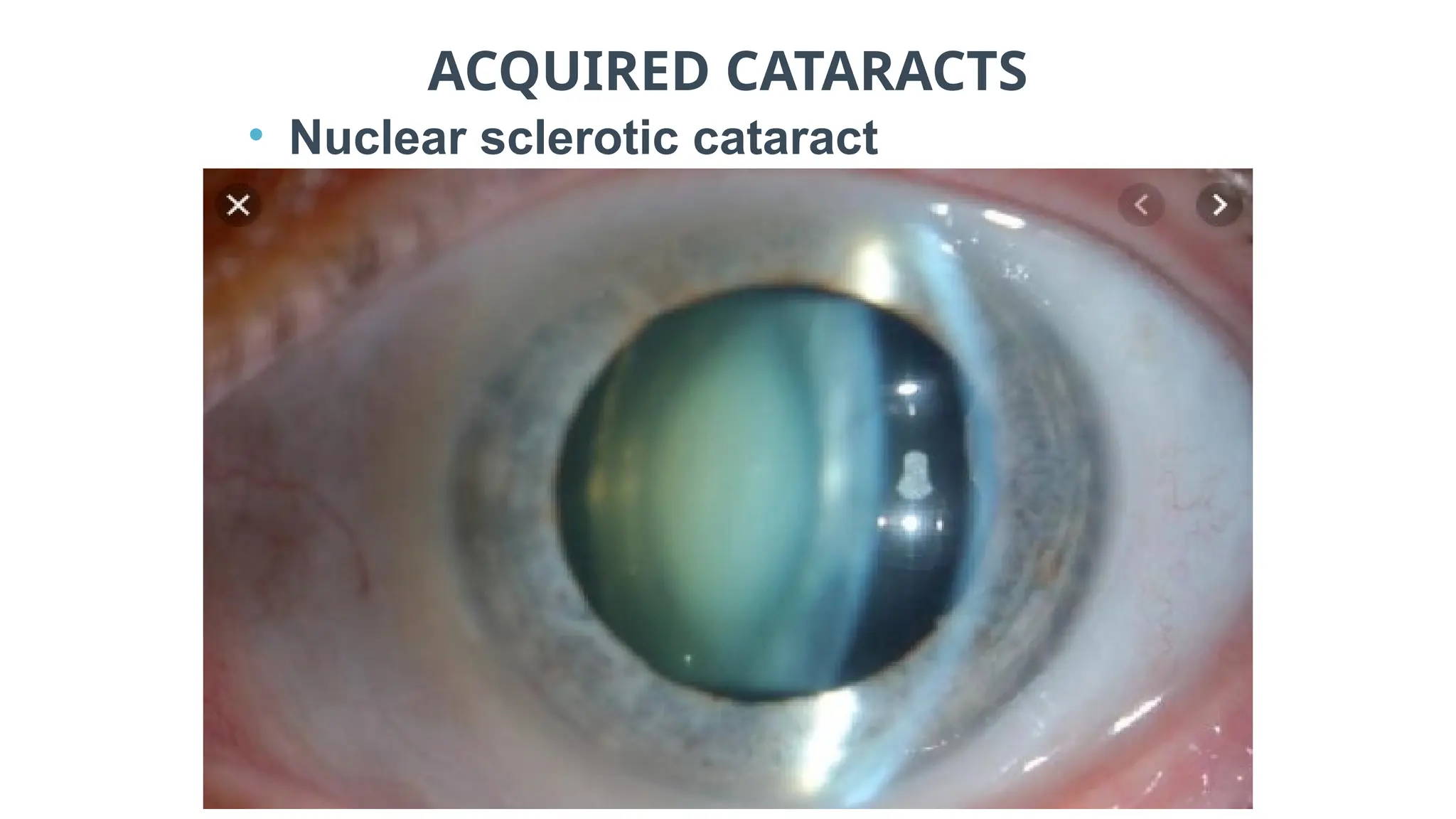
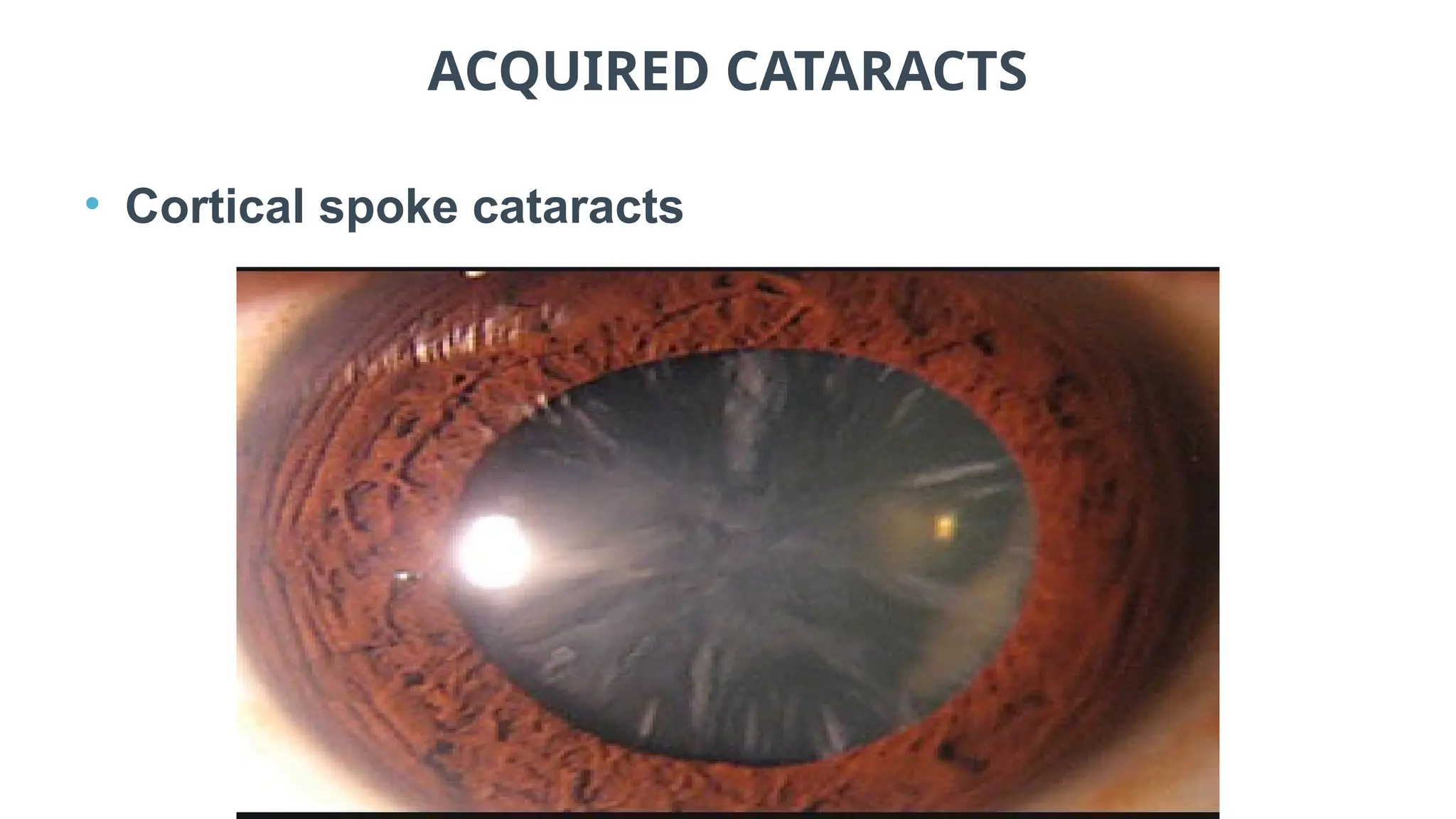
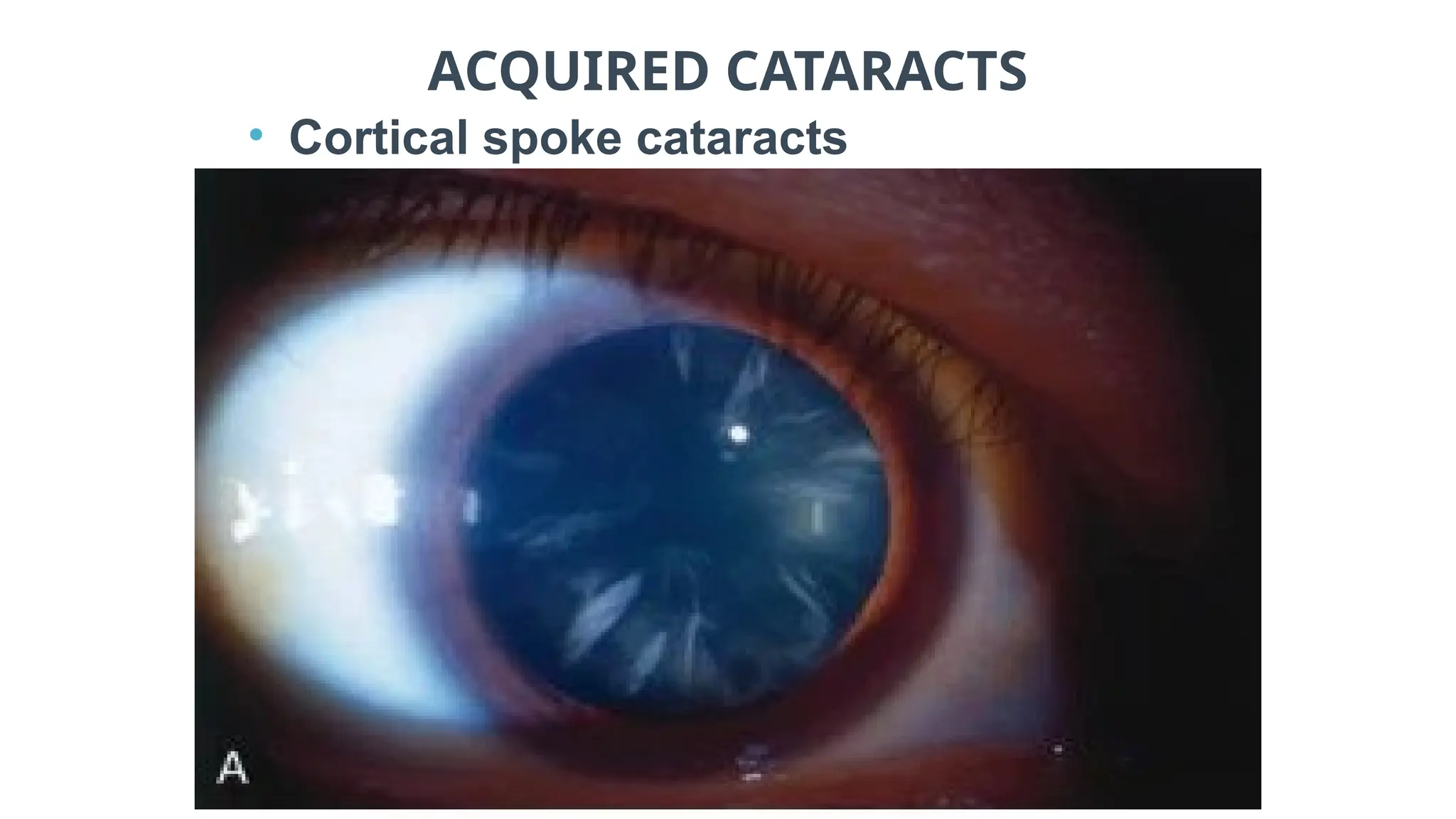
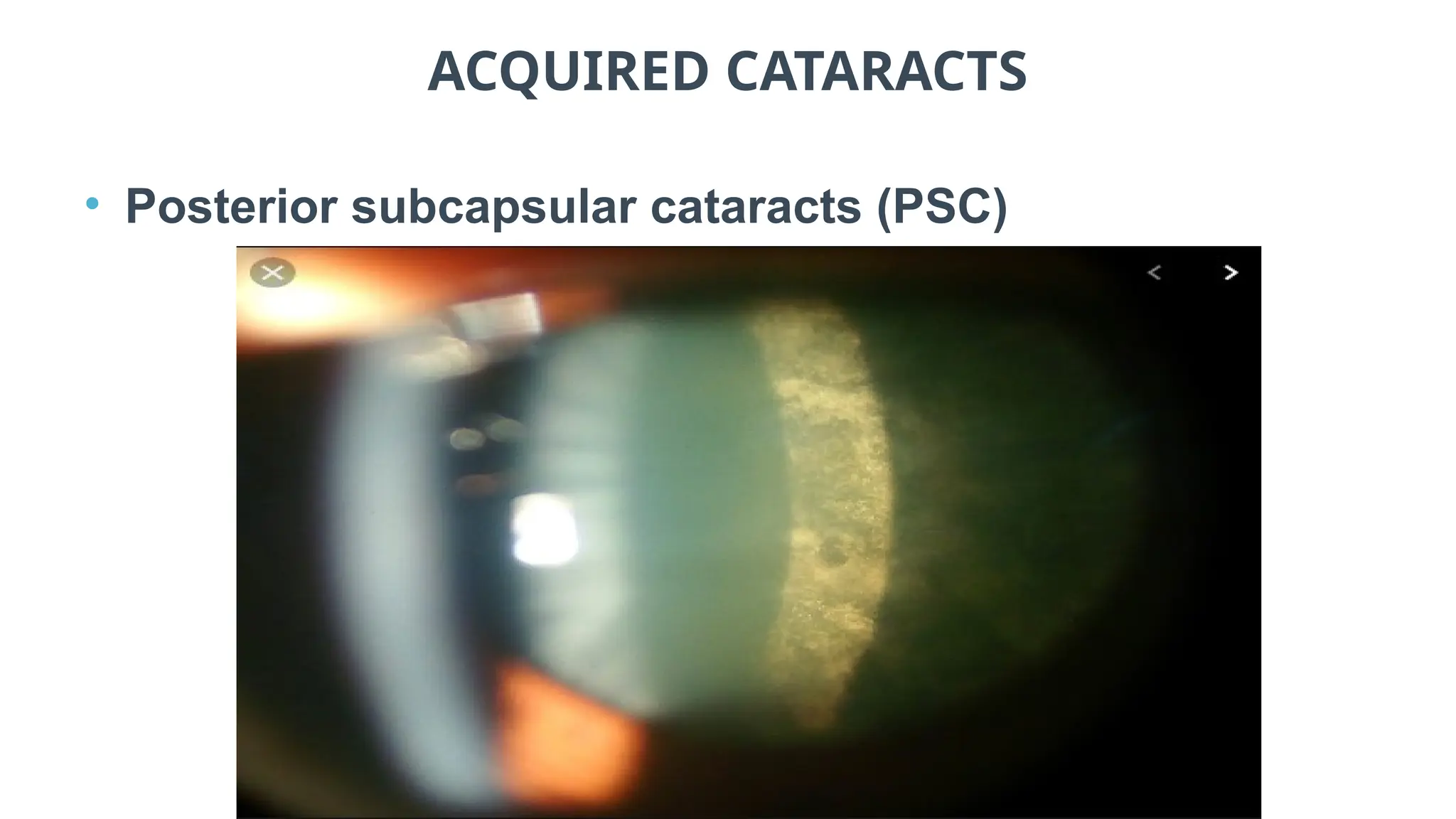
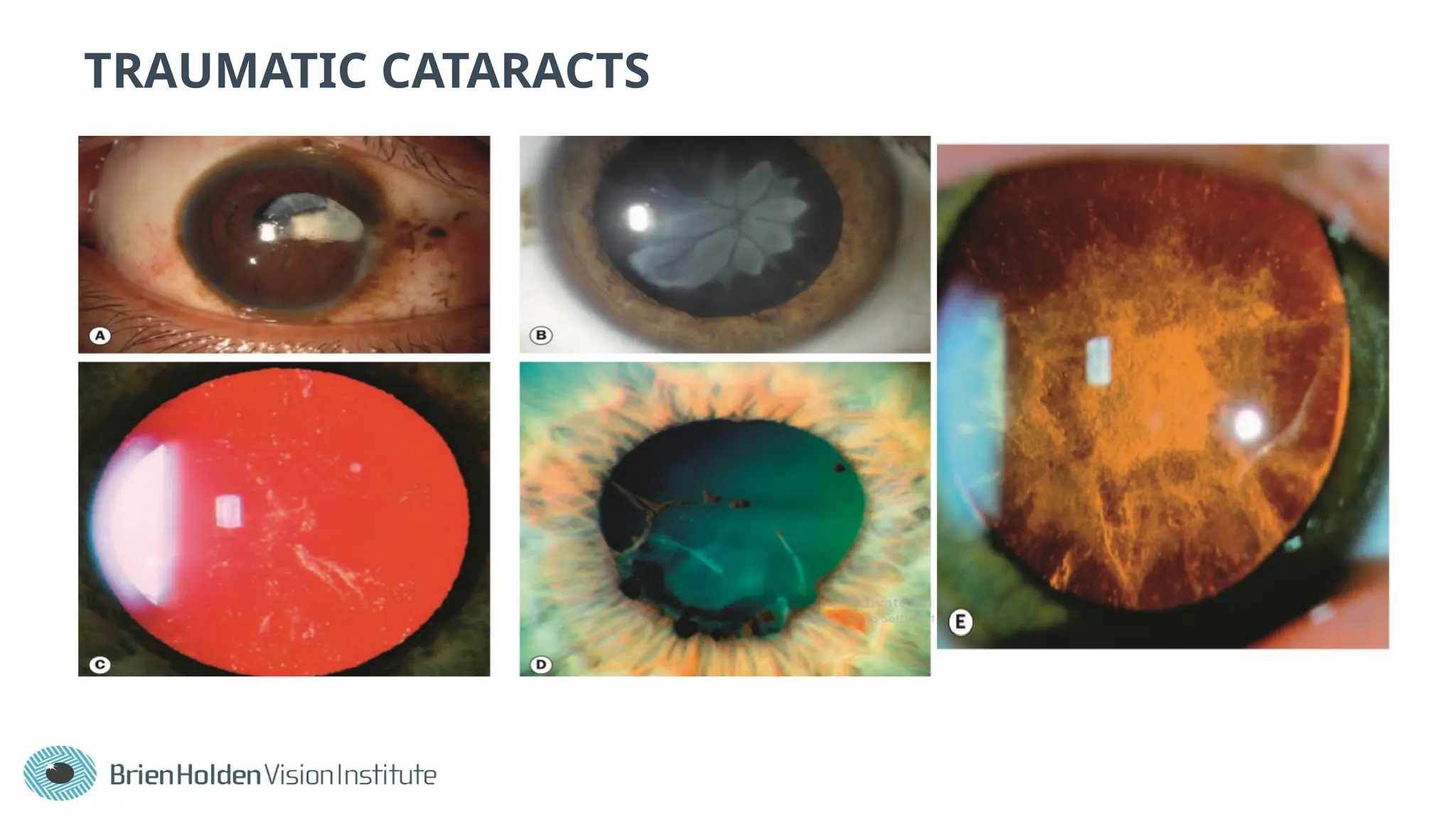
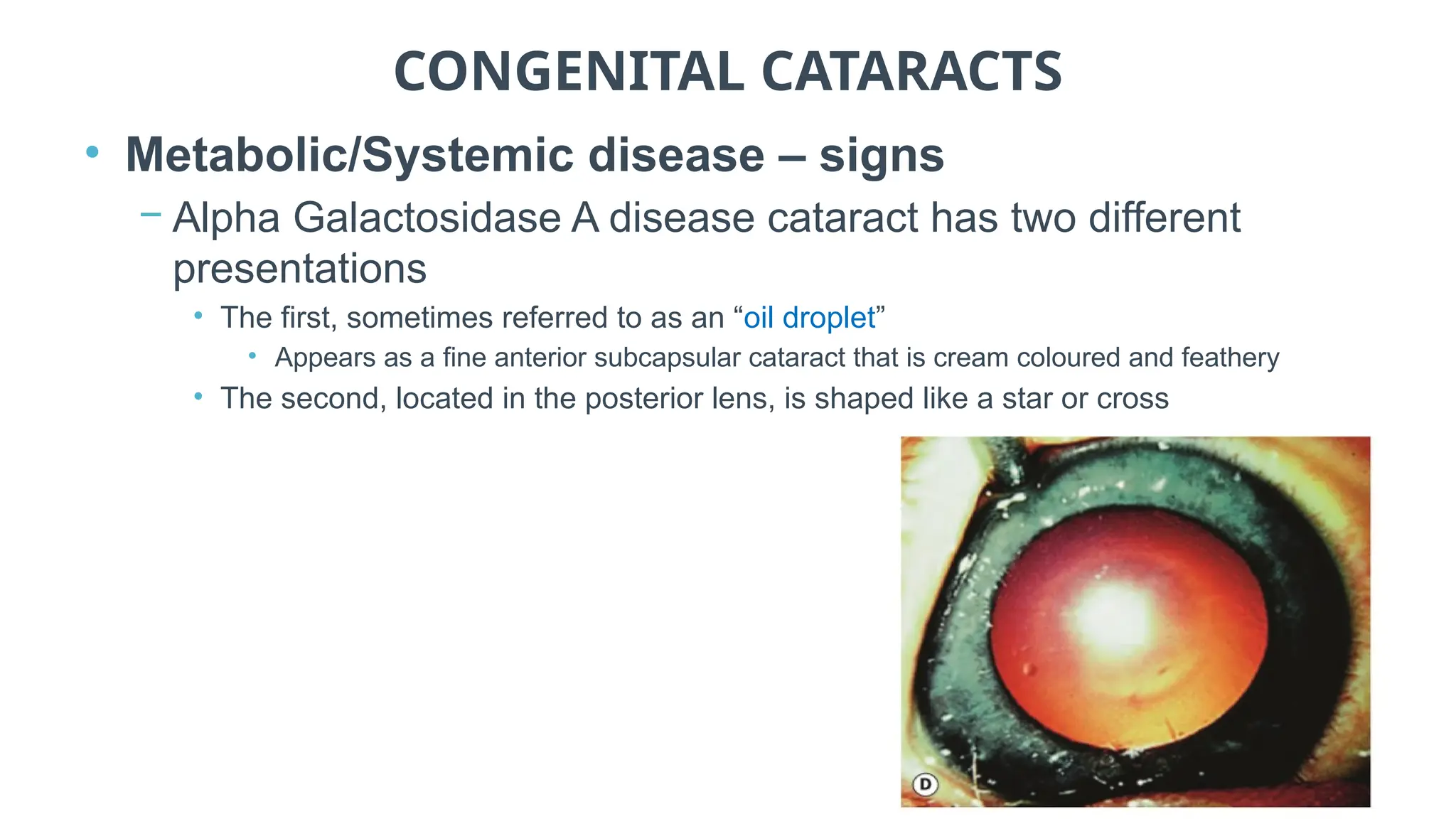
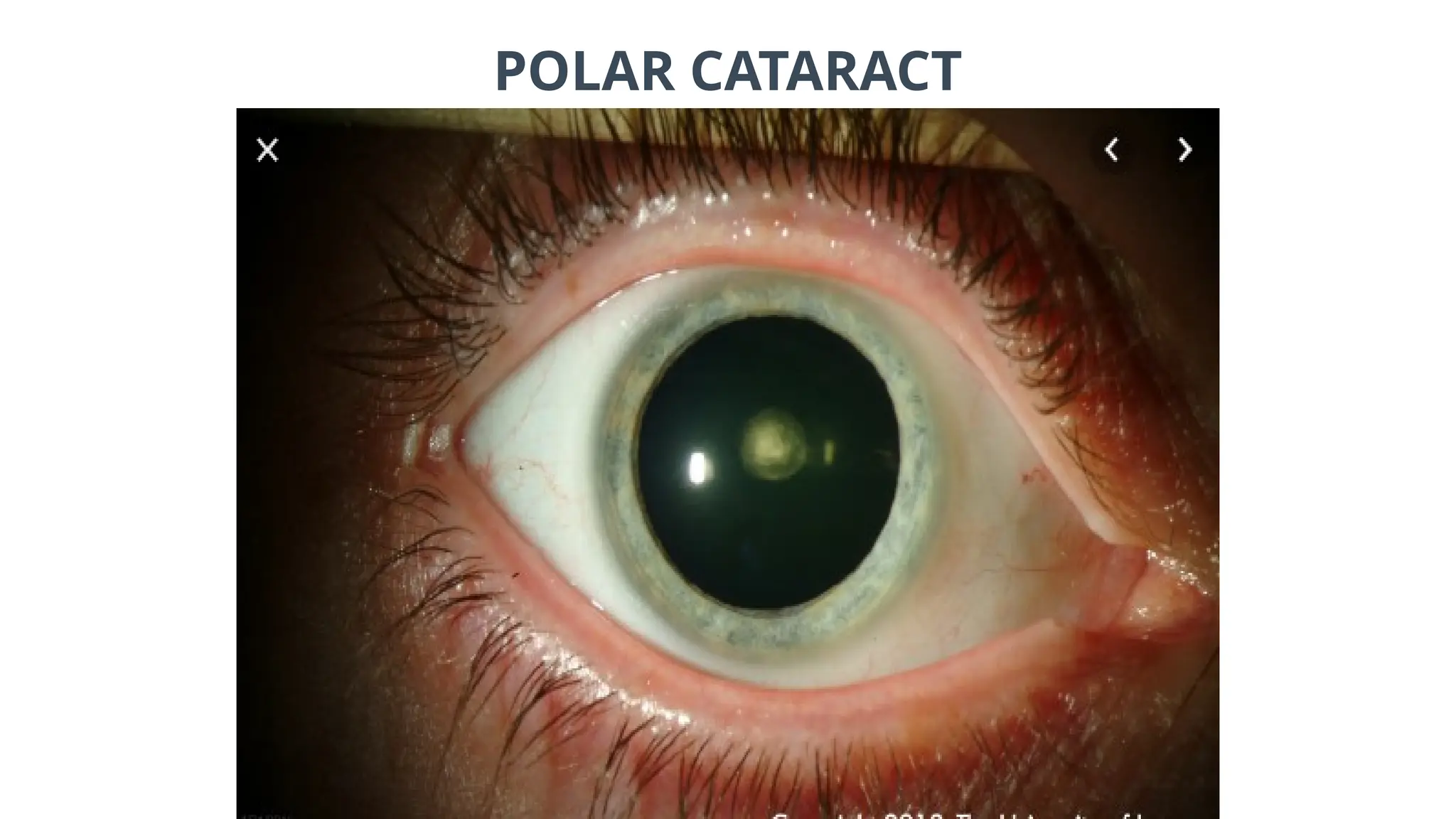
The document provides comprehensive insights into common eye disorders, specifically focusing on various types of cataracts—both acquired and congenital. It details methods of observation and assessment, symptoms, risk factors, and management plans for different cataract forms, highlighting critical factors such as age, family history, and exposure to certain conditions or medications. Additionally, it discusses the impact of lens abnormalities due to systemic diseases and the need for individualized treatment referrals based on visual function impairment.